// 6
Cocoon Training Manual Background
Those X rays that interact will do so by one of two methods, photoelectric absorption or Compton
scatter.
Photoelectric absorption
In photoelectric absorption, the incident X-ray energy is completely absorbed in the interaction me-
dium (e.g., tissue) and the X ray is removed from the beam and does not have the ability to scatter.
Compton scatter
With Compton scatter, the incident X ray scatters in the interaction medium and only a partial amount
of original energy is absorbed. The remaining energy goes to the scattered X ray. This scattered en-
ergy is therefore available to be absorbed else where, for example, in the technician.
During the process of photoelectric absorption or Compton scatter, energy is transferred to the
interaction medium. We quantify the eect of this energy absorption using a parameter called “ab-
sorbed dose”, i.e., the amount of energy absorbed for a given mass of absorbing medium. Someone’s
risk from radiation exposure is directly proportional to the dose they receive. The regulatory agen-
cies set limits on absorbed dose for workers and the general public to ensure that radiation risk is
kept as low as practical.
Biological Eects of Radiation
While X rays are an important part of the diagnostic process, it is important to be aware that there is
potential for biological damage to occur when exposed to ionizing radiation. Eorts should be made
to evaluate the benefit and potential risk in order to avoid unnecessary radiation exposure. The ben-
efits of medical/dental evaluation using X-ray technology are obvious, but the biological eects of
ionizing radiation must be weighed against the benefits. These eects are commonly grouped into
two categories:
Non-stochastic Eects (deterministic eects)
Non-stochastic eects related to those that are non-random and are directly related to the radiation
dose received. For these eects to occur, a threshold dose must be met. Once the threshold has been
exceeded, the severity of biological damage (e.g., skin burns, hair loss, reddening of the skin, cata-
racts) increases with the dose received. These eects are seen only after exposure to large doses of
radiation (> 1,000 mSv), much larger than doses received when undergoing dental imaging.
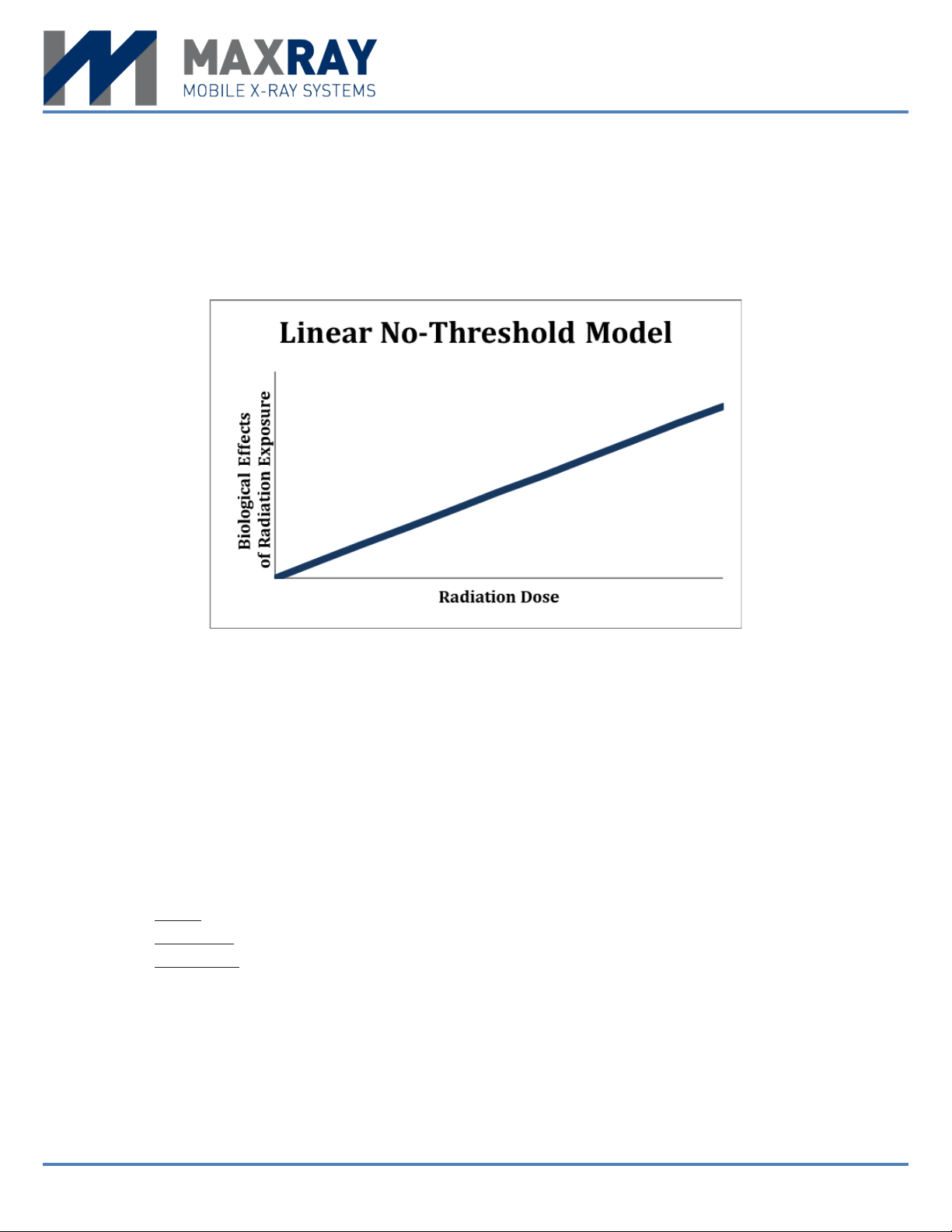
Stochastic Eects (probabilistic eects)
Stochastic eects are randomly occurring and the severity of biological damage (e.g., cancer, birth
defects) is independent of the dose received. Since it is based on probability, the chance of occur-
rence increases with radiation exposure. Stochastic eects are of typical concerned when speaking of
exposure to diagnostic X rays; radiation dose is very small; therefore, the only real potential outcome
is the random chance of cancer.