BATTERY OPERATION
The J1010 has an installed maintenance-free 12 volt NiMH rechargeable battery.
Please allow 10 hours to completely recharge the battery if drained fully. Recharge in
the AC operation mode: flip on the power switch at the back panel of the unit. Do not
press the ON/OFF button. DO NOT charge the battery for more than 24 continuous
hours. The unit may be left plugged in, but the power switch must be off to prevent
damage to the battery.
Battery charge status is indicated on the LED tracing screen (battery mode only).
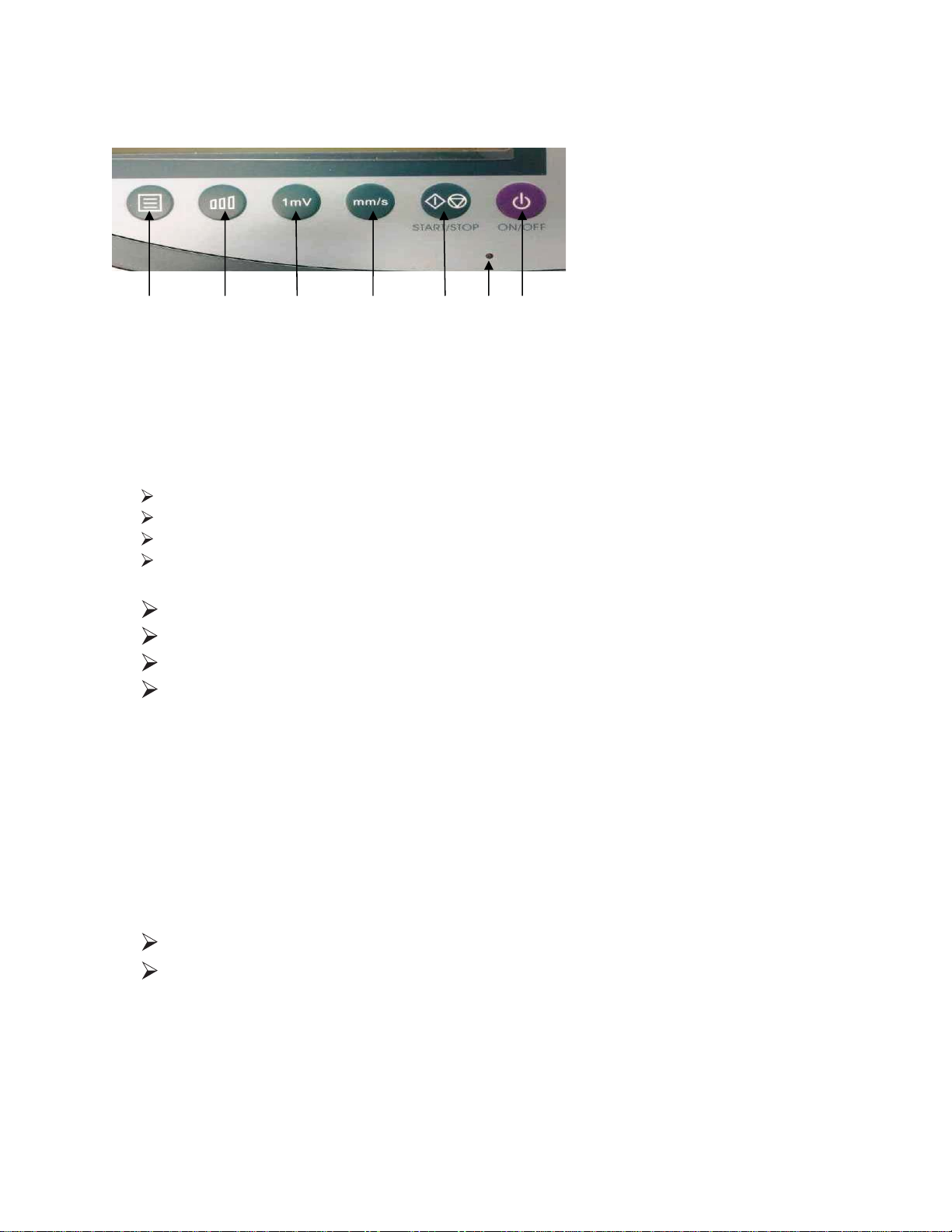
Indicator light flashes green on keypad when charging and turns to a solid green when
fully charged. Turn the power switch off at this time (Power switch on back panel of
unit solely operates battery charging).
To operate solely on battery turn power switch on back panel to OFF (battery icon
should be illuminated in upper right corner of screen). If battery icon is white battery is
fully charged and ready to use, battery icon will empty as battery is depleted.
The cardiograph will turn itself off after 5 minutes of non-use. Press ON/OFF to
resume. During long term storage or extended periods of non-use, recharge the battery
every 6 months.
Always check battery level on the screen before running on battery power.
LOADING THE ECG PAPER
Depress the button on the left side of the machine to open the door of the paper
cabinet, and lift door off. Load paper printed side down and replace the door with the
rubber roller sitting on top of the paper.
Avoid slack in the paper tension and align the paper straight with the door edge.
Adjust paper position as necessary if printing is off center. PAPER? alarm will appear
on screen until paper is replaced or the situation is remedied.
PlacepaperinECGslotgridfacing
down.
Placecoverovertopofpaper
andclose.
ECGreadytoprint
5