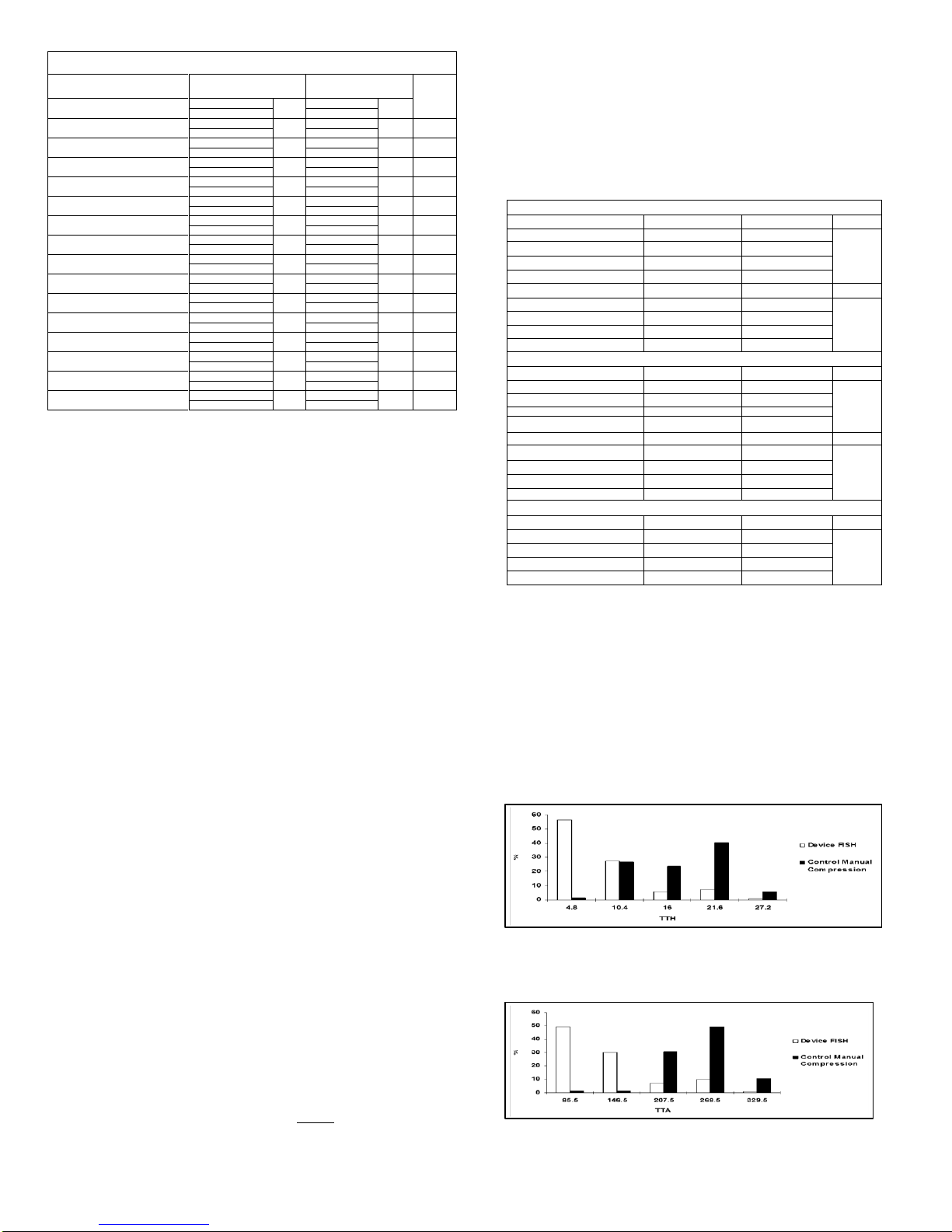
Table 1 –Major and Minor Complications through 30 Days –Diagnostic ITT Patients
Cumulative Major and Minor Complications –Blackwater Test for Equivalence
Randomized Subjects N = 206
Combined Major Complications
Access-site related bleeding requiring transfusion
New ischemia in ipsilateral leg
Vascular surgical repair, US-guided compression,
Transcatheter embolization, or stent graft
Surgery for access-site related nerve injury
Permanent access-site related nerve injury
Access-site related infection requiring IV
antibiotics and/or extended hospitalization
Combined Minor Complications
Access-site related hematoma > 6cm
Pseudoaneurysm treated with ultrasound-guided
thrombin injection
Pseudoaneurysm treated with ultrasound-guided
fibrin adhesive injection
Non-treated pseudoaneurysm (documented by
ultrasound)
Non-treated AV fistula (documented by
ultrasound)
* Exact 95% confidence interval based on Clopper-Pearson method
** Blackwater’s test with an equivalent limit of 0.05. The significance level of 0.041 was used for the interim
*** Device Success –the ability to achieve hemostasis without major adverse events of the use of mechanical compression and
within the allotted time (60 minutes).
**** Procedure Success –the ability to establish hemostasis in a given subject within any time period using any method.
Table 1 shows that the overall MACE rates were 0.72% and 0.0% for FISH™ device and control group, respectively.
The overall Minor Adverse Event rates were 2.88% and 1.5% for the FISH device and control group respectively.
Clinical Studies
The FISH closure device was studied in an open-label, randomized, multi-center clinical trial which enrolled 297
diagnostic and interventional patients. This United States based trial evaluated the FISH device to manual
compression. The study included both diagnostic (N=206) and interventional (N=91) patients requiring a
procedure with and 8Fr or smaller sheath size. The study of interventional patients with the FISH™ device is
currently ongoing. Data from the interventional study is not discussed here. Each investigator had the
opportunity to enroll up to 2 roll-in patients which were non randomized patients. There were a total of 28 roll-in
patients combined in the diagnostic and interventional study. The patients were randomized on a 2 to 1
randomization scheme (FISH™ device vs. manual compression). Of the 206 diagnostic patients enrolled in the
study, 139 received the FISH™ device and 67 received manual compression.
This study included 8 U.S. sites and enrolled patients between January 2004 and June of 2006. There were a
total of 40 investigators which enrolled patients for the study.
All patients enrolled in the study provided a signed written informed consent and agreed to return for a follow-up
evaluation at 30 ± 5days. The study included patients who were undergoing diagnostic or therapeutic coronary or
peripheral procedure performed percutaneously via the common femoral artery. The candidates were required
to meet general inclusion and exclusion criteria. The patients did not require a femoral artery angiogram prior to
placement of the FISH Device.
The null hypothesis for safety was that the experimental device had a major adverse event rate that exceeded
that of the control by a delta of 5%. The alternate hypothesis was that the experimental device has a primary
safety endpoint rate less than that of the control or exceeding that of the control by no more than the delta 5%.
Null Hypothesis
MII FISH (%MACE) > Manual Compression (%MACE) + 5% delta
Alternative Hypothesis
MII FISH (%MACE) < Manual Compression (%MACE) + 5% delta
For the diagnostic patients, the FISH device demonstrated safety with a total adverse event rate of 0.7% (1/139)
versus the control 0.0% (0/67). The one event for the FISH device was a site related bleeding requiring
transfusion. These rates for MACE in the diagnostic patients were found to be equivalent (p < 0.0001) under the
experimental conditions outlined prospectively in the investigational plan.
The minor adverse event rate was low for both the FISH device (2.9%) and the control (1.5%), the tests for
equivalence showed these to be equal (p=0.039). The events for the device include 3 hematomas > 6cm and 1
Pseudoaneurysm. For the control there was one hematoma > 6cm. During the course of this clinical trial there
was one patient death (1 FISH, 0 Manual Compression). The death was not related to the use of the device.
There were no Unanticipated Access Site Related Adverse Events.
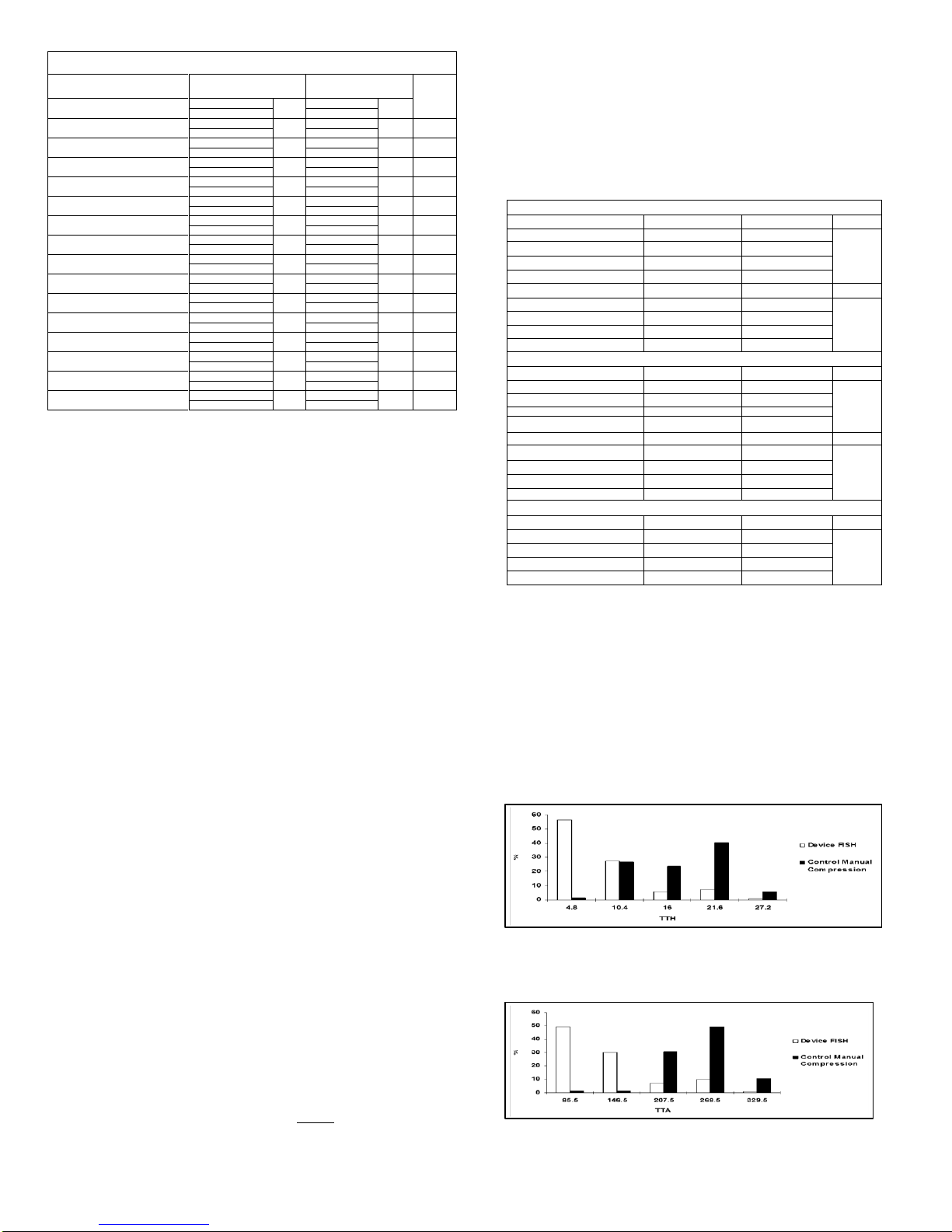
Effectiveness Results
In all effectiveness endpoints the FISH device proved superior in diagnostic patients compared to the control
manual compression. The median time for hemostasis in the FISH patients was 6 minutes versus 17 minutes for
the control group manual compression. The median time for ambulation for the FISH device was 2.0 hours for the
FISH group versus 4.2 hours for the control. The median time to eligible discharge for the FISH device was 2.3
hours versus 4.5 hours for the control. The median time to eligible discharge for the FISH device was 2.3 hours
versus 4.5 hours for the control manual compression. The median time to discharge was 3.0 hours for the FISH
patients versus 4.9 hours for the control group manual compression. The following table (Table 2) shows the
effectiveness results.
Table 2 –Diagnostic Procedures: Primary Effectiveness Results ITT
Time to Hemostasis (Minutes)
Time to Ambulation (Hours)
Time to Eligible Discharge (Hours)
Time to Discharge (Hours)
Equivalence Study At 30 Day s
Discomfort (Subjective Scale 0-10)
The effectiveness calculations were based on the Wilcoxon Two-Sample Test using a normal approximation and two-sided criteria
(Pr > Z< .0001).
The results of the statistical analyses demonstrate that the FISH™ device is superior to Manual Compression in
terms of effectiveness measures for vascular hemostasis, ambulation, eligible discharge, discharge and
equivalent relative to discomfort subjectively measured at 30 days post procedure. The FISH device has
demonstrated safety through its low incidence of complications in diagnostic patients when compared to manual
compression.
Effectiveness Endpoints
Time to Hemostasis (TTH) was measured from the time of introducer sheath pull to the time the patient
achieved hemostasis. For this study, the time of hemostasis was defined as “Absence of oozing blood that is
readily treated by light compression methods (e.g. sandbags, pressure dressing, light manual pressure)”. The
study was designed to demonstrate TTH superiority as compared to the control therapy.
Figure 1 Histogram of Percentage of Patients vs. Time to Hemostasis (in minutes)
Time to Ambulation (TTA) –this was measured from the time of introducer sheath removal to the time when
the patient stood at the bedside and walked at least 20 feet without evidence of re-bleeding. The study was
designed to demonstrate TTA superiority as compared to the control therapy.
Figure 2 Histogram of Percentage of Patients vs. Time to Ambulation (in minutes)
Time to Eligible Discharge (TTED) –this was measured from the time of introducer sheath pull to the time when
the patient was deemed eligible for discharge from the hospital based only on the condition of the access site.
The study was designed to demonstrate TTED superiority as compared to the control therapy.