6
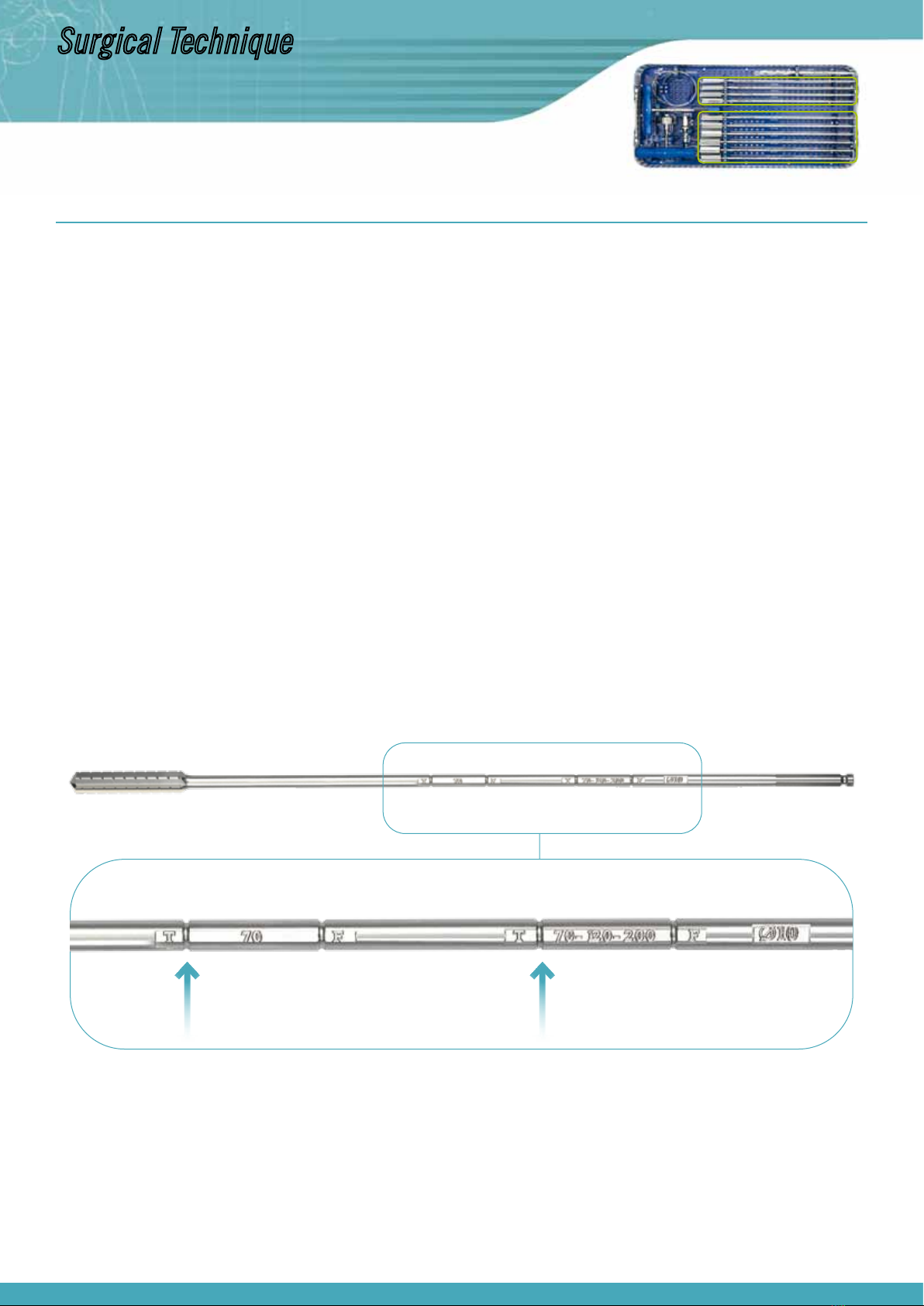
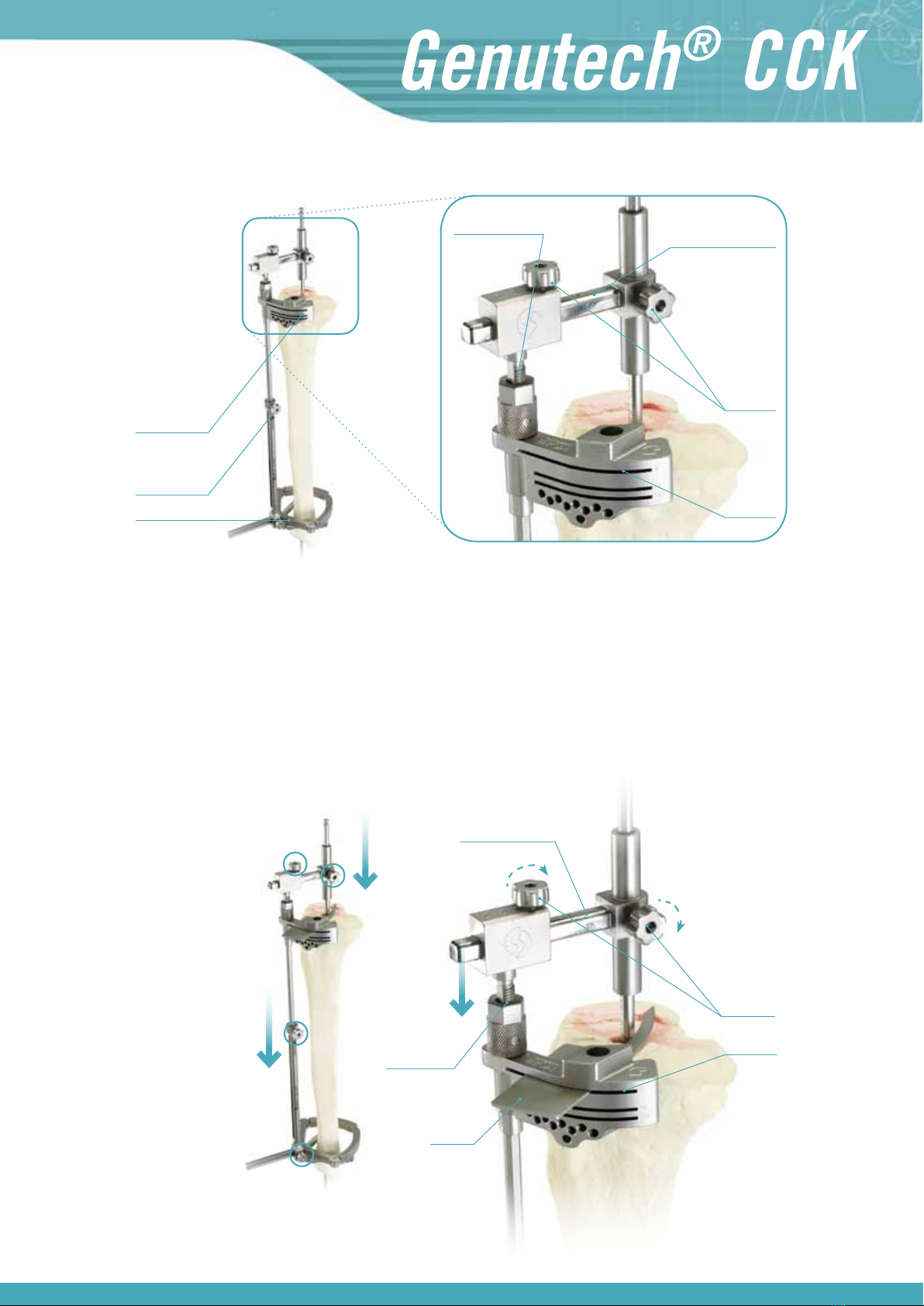
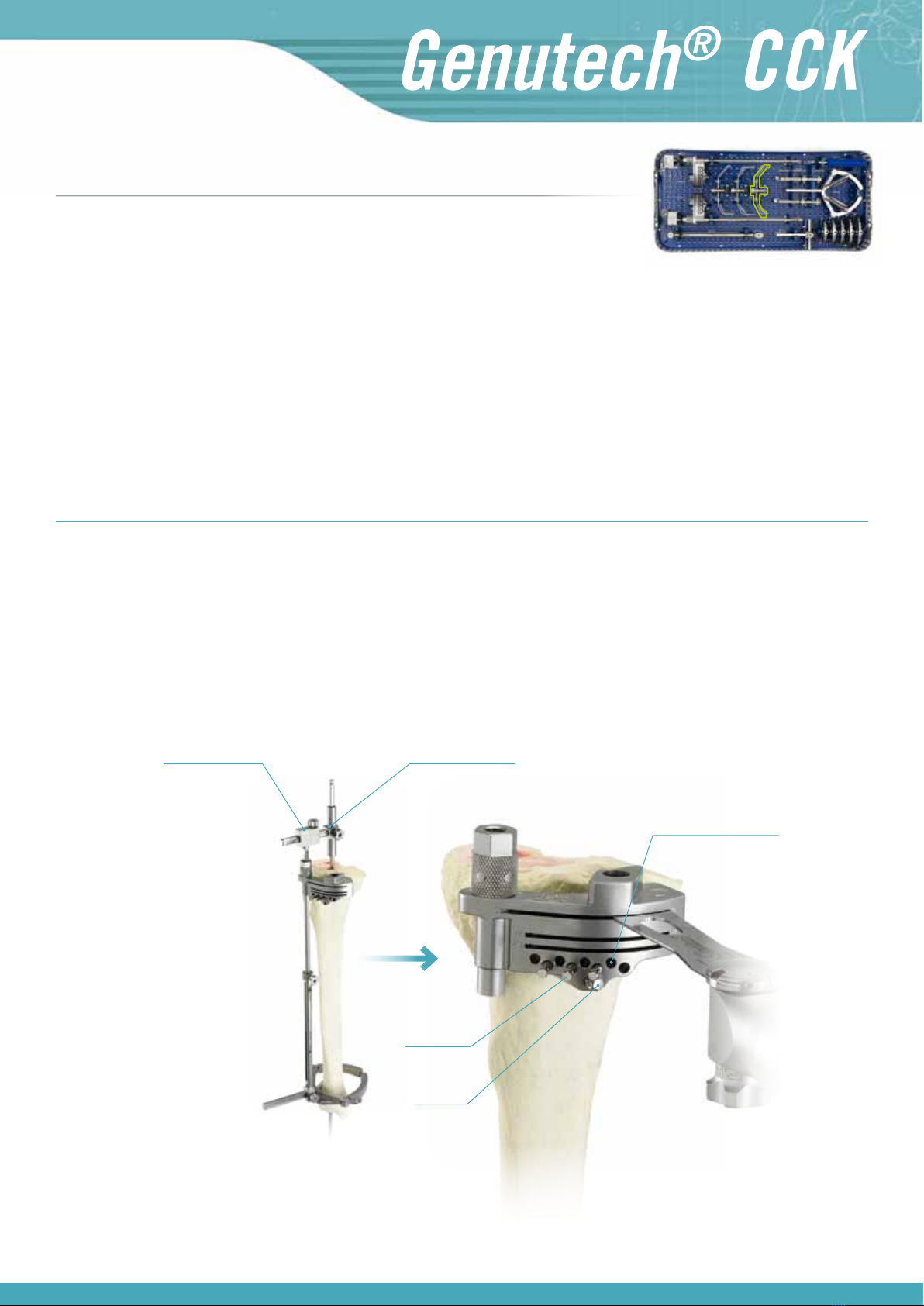
Installation of the revision probe of 0-8 or 0-12 mm
In the most favourable cases, where you only need to make a thin cut to sanitise the tibial
surface, with the “0” end (short arm) of the probe, look for the most depressed area of the
tibial plateau to ensure that the cut being made is always below said point. To do this you
must use the threaded displacement measuring system to move it down until it rests on said
area. Once the most depressed area has been reached, fix the tibial cutting guide and then
make the cut.
In extreme cases, in which the tibia is extremely damaged, a prosthesis has been replaced
with supplements or it is necessary to sanitise a bone which is significantly (8 mm, 12 mm,
etc.). Using supplements, in the medial, lateral or even the bilateral area, proceed as follows:
The ”0” end (short arm of the tibial probe) must be directed towards the most depressed
area of the most prominent tibial plateau. To do this you must use the threaded displacement
measuring system to move it down until it is rests on said area.
Then note down the amount of millimetres which the system has gone down (see measure-
ment on the graduated marks on the telescopic guide).
With the arm of the rod in position “8” or “12” probe the most depressed area of the plateau
with the most wear, and the following situations may arise:
a) The 8 mm arm of the “0-8” probe does not fit
In this case cut to +8 and install an 8 mm tibial supplement below the tibial tray
on that side.
b) The 8 mm arm is not in contact
In this situation, assemble the “0-12” probe, trying to ensure contact with its
12 mm arm, and the following situations may arise:
b1) The 12 mm arm does not fit, leaving two options:
· Move it down with the sheave of the tibial cutting guide until the 8 mm arm
touches the area with the most wear, making a +8 mm recut in that area. In this
situation there will be additional displacement with the sheave to transfer it to
the thickness of the tibial insert (to maintain the interline), and an 8 mm tibial
supplement will be used in the aforementioned most depressed area.
· Keep the cutting guide in its initial position and recut +12 on the plateau with
most wear, using a 12 mm tibial supplement.
b2) The 12 mm arm is not in contact
Move down the threaded displacement measuring system to the 12 mm arm, ma-
king a +12 recut in the most depressed area to use a 12 mm tibial supplement.
You must also take into account the amount of millimetres which the cutting guide
has moved downwards with the threaded displacement system and add them to
the thickness of the tibial insert and ensure that the interline is maintained. Note:
Move the system down until the probe touches the ti-
bial plateau.
Surgical Technique
Set 1. Upper tray