Warning: Splitting the lumens beyond this point may result in
excess tunnel bleeding, infection, or damage to the catheter
lumens.
Note: A tunnel with a wide gentle arc lessens the risk of kinking. The
tunnel should be short enough to keep the extension set of the catheter
from entering the exit site, yet long enough to keep the cuff 2cm
(minimum) from the skin opening.
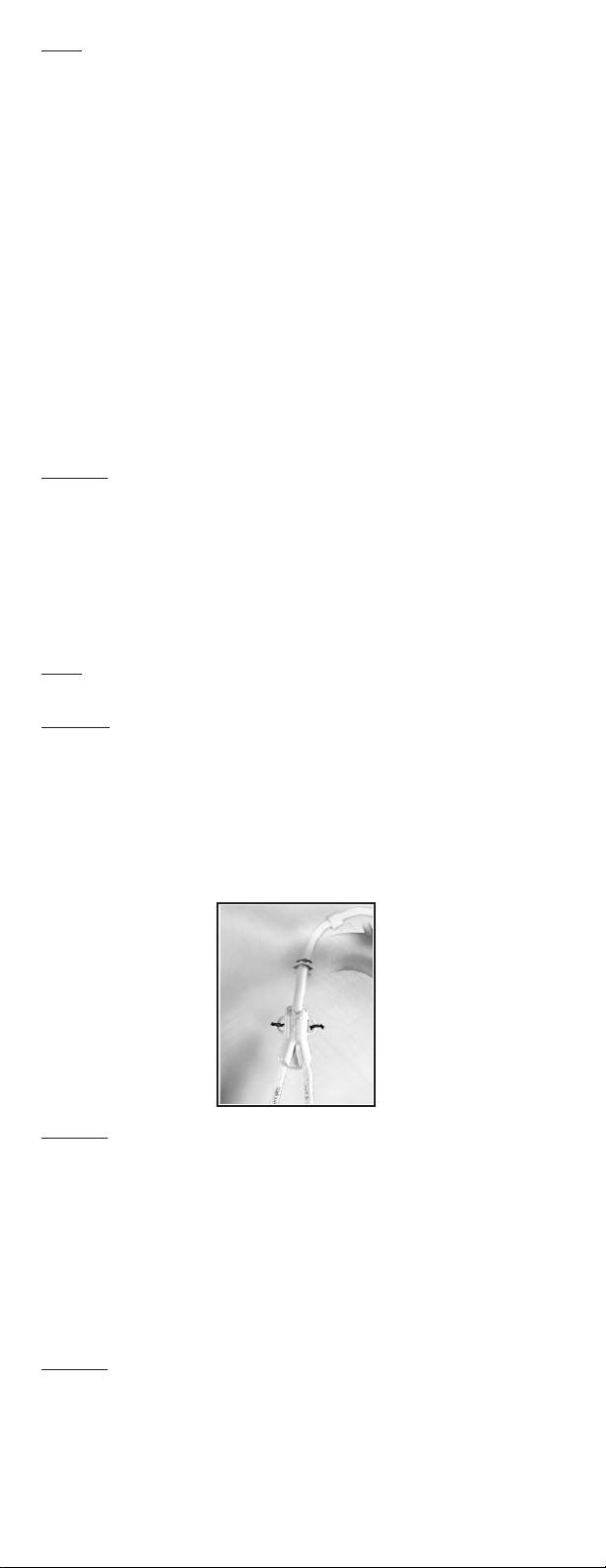
16. Irrigate catheter with saline, then clamp catheter extensions and
white secondary clamps to assure that saline is not inadvertently
drained from lumens. Use clamps provided.
INSERTION:
17. Insert the introducer needle with attached syringe, or into the
target vein. Aspirate to insure proper placement.
18. Remove the syringe, and place thumb over the end of the needle to
prevent blood loss or air embolism. Draw exible end of guidewire
back into advancer so that only the end of the guidewire is visible.
Insert advancer’s distal end into the needle hub. Advance guidewire
with forward motion into and past the needle hub into the target
vein.
Caution: The length of the wire inserted is determined by the size of the
patient. Monitor patient for arrhythmia throughout this procedure. The
patient should be placed on a cardiac monitor during this procedure.
Cardiac arrhythmias may result if guidewire is allowed to pass into the
right atrium. The guidewire should be held securely during this
procedure.
19. Remove needle, leaving guidewire in the target vein. Enlarge
cutaneous puncture site with scalpel.
20. Thread dilator(s) over guidewire into the vessel (a slight twisting
motion may be used). Remove dilator(s) when vessel is sufciently
dilated, leaving guidewire in place.
Caution: Insufcient tissue dilation can cause compression of the
catheter lumen against the guidewire causing difculty in the insertion
and removal of the guidewire from the catheter. This can lead to
bending of the guidewire.
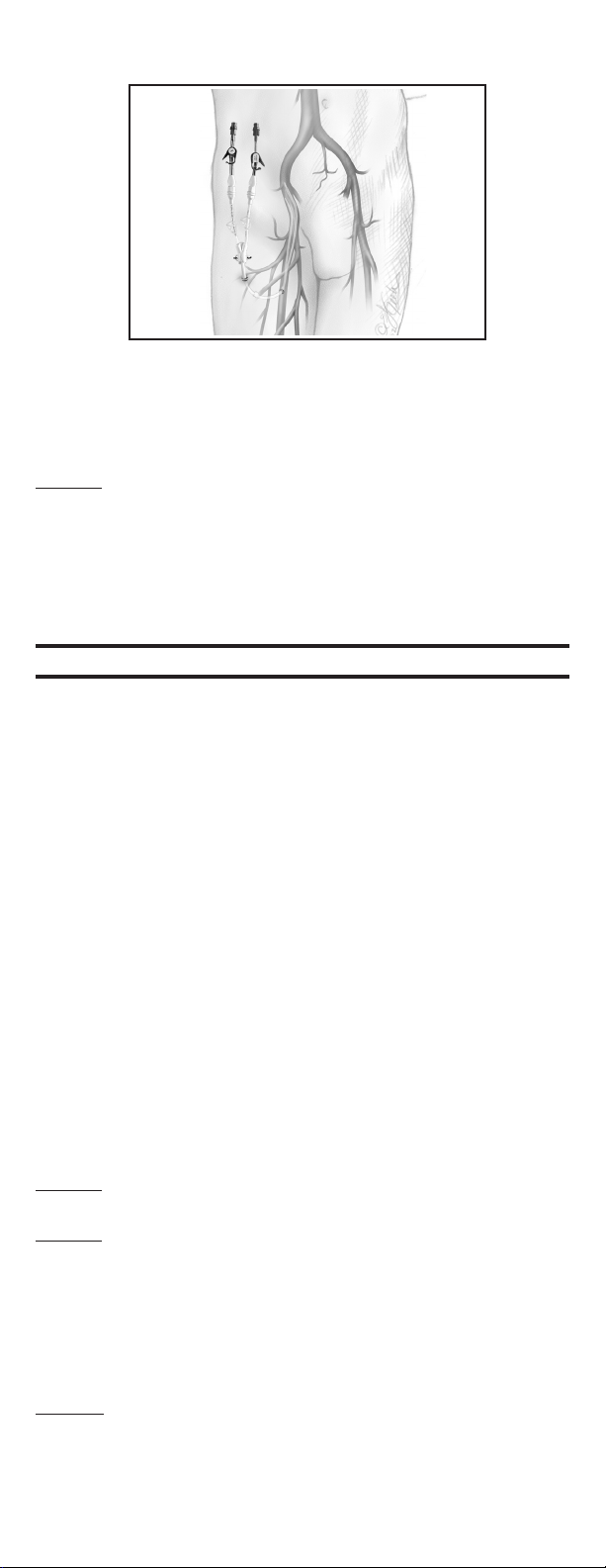
21. Thread Vascu-Sheath®Introducer over the proximal end of the
guidewire. Once the Vascu-Sheath®Introducer is in the target vein,
remove the guidewire leaving the sheath and dilator in position.
Warning: Do NOT bend the sheath/dilator during insertion as bending
will cause the sheath to prematurely tear. Hold sheath/dilator close to
the tip (approximately 3cm from tip) when initially inserting through the
skin surface. To progress the sheath/dilator towards the vein, regrasp
the sheath/dilator a few centimeters (approximately 5cm) above the
original grasp location and push down on the sheath/dilator. Repeat
procedure until sheath/dilator is fully inserted.
Warning: Never leave sheath in place as an indwelling catheter. Damage
to the vein will occur.
22. Install end cap over dilator opening to prevent blood loss or air
embolism.
23. Remove dilator and end cap from sheath.
24. Insert distal tips of catheter into and through the sheath until
catheter tips are correctly positioned in the target vein.
25. Remove the tear-away sheath by slowly pulling it out of the vessel
while simultaneously splitting the sheath by grasping the tabs and
pulling them apart (a slight twisting motion may be helpful).
Warning: Do NOT pull apart the portion of the sheath that remains in
the vessel. To avoid vessel damage, pull back the sheath as far as
possible and tear the sheath only a few centimeters at a time.
26. Make any adjustments to catheter under uoroscopy. The distal
venous tip should be positioned at the level of the caval atrial
junction or into the right atrium to ensure optimal blood ow.
-6-