Part Number: PIB01054 Page 5 of 18
Revision: A Revision Date: June 2020
increased when these lenses are worn overnight. Studies have shown that contact lens wearers who are
smokers have a higher incidence of adverse reactions than nonsmokers. If a patient experiences eye
discomfort, excessive tearing, vision changes, or redness of the eye, the patient should be instructed to
immediately remove lenses and promptly contact his or her Eye Care Practitioner.
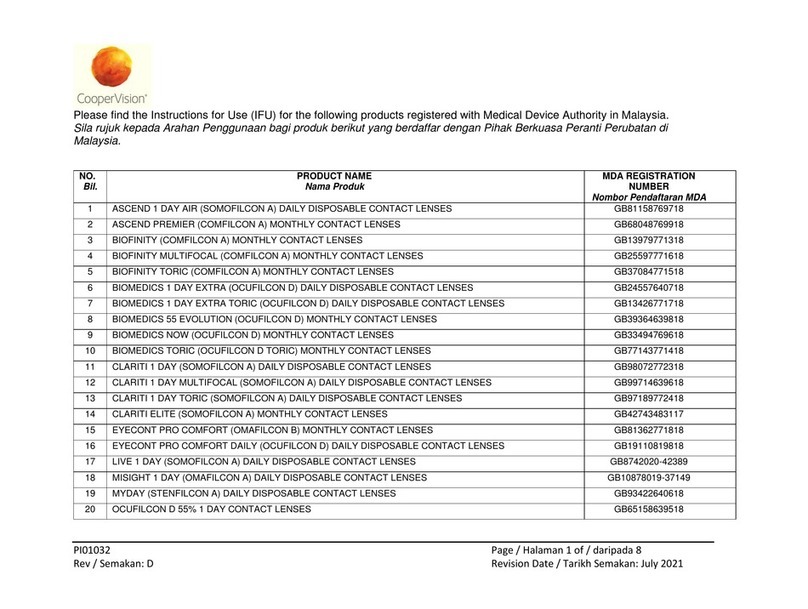
The results of a study3indicate the following:
a. The overall annual incidence of infected corneal ulcer (ulcerative keratitis) in daily wear contact
lens users is estimated to be about 4.1 per 10,000 persons and about 20.9 per 10,000 persons in
extended wear contact lens users.
b. The risk of infected corneal ulcer (ulcerative keratitis) is 4 to 5 times greater for extended wear
contact lens users than for daily wear users. When daily wear users who wear their lenses overnight
and extended wear users who wear their lenses on a daily basis are excluded from the comparison,
the risk among extended wear users are 10 to 15 times greater than among daily wear users.
c. When daily users wear their lenses overnight (outside the approvedindication), the risk ofulcerative
keratitis is 9 times greater than among those who do not wear them overnight.
d. The overall risk of infected corneal ulcer (ulcerative keratitis) may be reduced by carefully following
directions for lens care, including cleaning the lens case.
e. The risk of infected corneal ulcer (ulcerative keratitis) among contact lens users who smoke is
estimated to be 3 to 8 times greater than among non-smokers.
f. If you experience eye discomfort, excessive tearing, vision changes, redness of the eye or other
problems, you should be instructed to immediately remove your lenses and promptly contact your
Eye Care Practitioner. It is recommended that you see your Eye Care Practitioner routinely as
directed.
5. PRECAUTIONS
Handling Precautions:
•Do not use if the sterile blister package is opened or damaged.
•Always wash and rinse hands before handling lenses. Do not get cosmetics, lotions, soaps, creams,
deodorant, or sprays in the eyes or on the lenses. It is best to put on lenses before putting on makeup.
Water-based cosmetics are less likely to damage lenses than oil-based products.
•Lens damage may occur if you handle your lens with dirty hands.
•Carefully follow the handling, insertion, removal, cleaning, and wearing instructions prescribed by your
Eye Care Practitioner.
•Always handle lenses gently and avoid dropping them.
•Never use tweezers or other tools to remove lenses from the lens container. Pour the lens and
packaging solution into your hand.
•Do not touch the lens with fingernails.
Lens Wearing Precautions:
•Never wear your lenses beyond the period recommended by your Eye Care Practitioner.
•If aerosol products such as hairspray are used while wearing lenses, be careful and keep eyes closed
until the spray has settled.
•Avoid all harmful or irritating vapors and fumes while wearing lenses.
•Ask your Eye Care Practitioner about wearing the lenses during sporting activities.
3New England Journal of Medicine, September 21,1989;321(12),pp.773-783