Allergan TrueTear Owner's manual

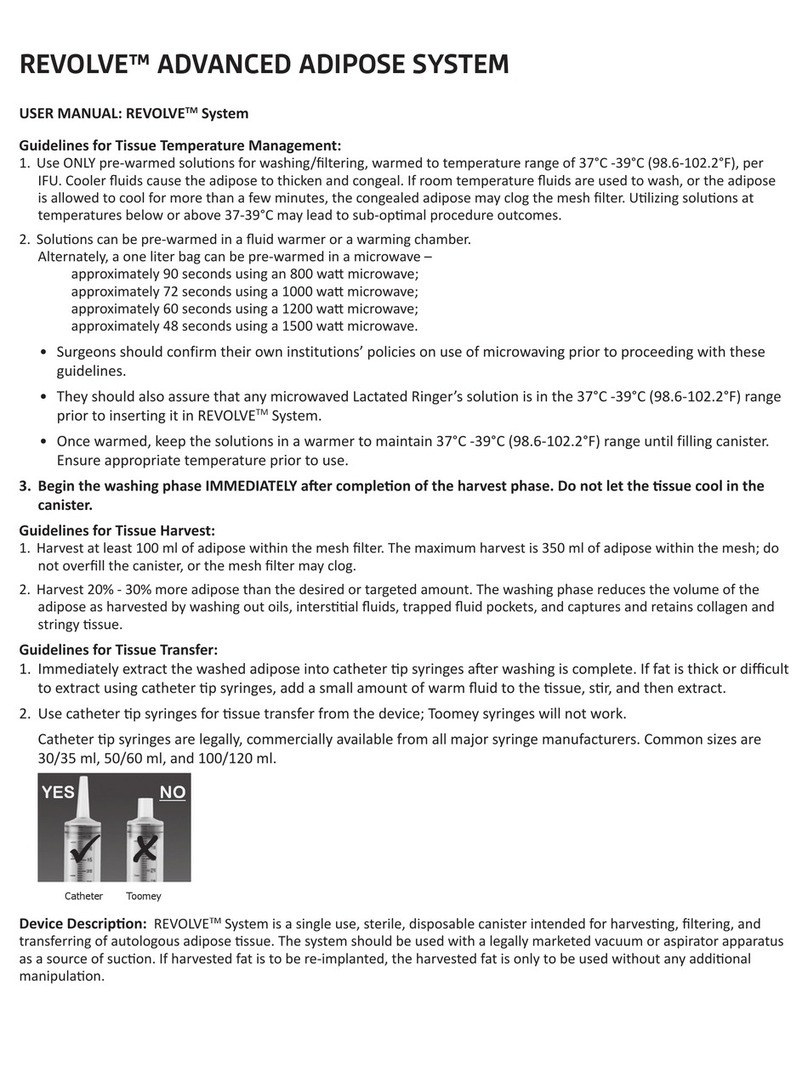
TrueTear®Intranasal Tear Neurostimulator
Professional Information Guide
Rx Only—Federal law restricts this device to sale by or on the
order of a physician or properly licensed practitioner.
Proper patient training on use of the device is required before
home use.
1 INDICATIONS FOR USE
The TrueTear®Intranasal Tear Neurostimulator (TrueTear®device) provides a temporary
increase in tear production during neurostimulation to improve dry eye symptoms in adult
patients with severe dry eye symptoms.
2 CONTRAINDICATIONS
The patient should not be prescribed the device if they have any of the following (these
contraindications are also provided in the patient labeling):
• A cardiac demand pacemaker, implanted or wearable defibrillator, or other
implanted metallic or electronic device in the head or neck
• A known hypersensitivity to the hydrogel device material that contacts the
nasal mucosa
• Chronic or recurrent nosebleeds, a bleeding disorder, or another condition that
can lead to increased bleeding
3 WARNINGS
The patient should be warned of the following (these warnings are also provided in the
patient labeling):
• Only apply stimulation in a manner consistent with the instructions in
this document.
• Do not apply stimulation in the presence of electronic monitoring equipment
(eg, cardiac monitors, ECG alarms), which may not operate properly when the
electrical stimulation device is in use.
• Do not apply stimulation when in the bath or shower.
• Do not apply stimulation while driving, operating machinery, or during
any activity in which sneezing or watery eyes may put the user at undue risk
of injury.
• Do not apply the device to the neck, chest, or areas other than the nose.
• Persistent use of stimulation in the presence of irritation of the target nasal
tissue may cause injury.
• Operation in close proximity (eg, 3 feet or less) to shortwave or microwave therapy
equipment may produce instability in the output of the device.
• Do not use the device in the presence of a flammable anesthetic mixture with air or
with oxygen or nitrous oxide as there is a remote possibility (comparable to the risk
of a mobile phone) it could ignite the gas.
• The TrueTear®device is limited only to the improvement in dry eye symptoms
as the safety and effectiveness in the treatment of dry eye disease has not been
established.
• In the pivotal clinical study, the safety and effectiveness of intranasal electrical
stimulation was characterized over a 6-month period of time. The safety and
effectiveness of the device for longer periods of use has not been established.
Periodic evaluation of the nasal cavity is recommended if the device is to be used
over a longer period of time.
• The clinical studies were not designed to evaluate any changes in nerve sensitivity.
• The safety of intranasal electrical stimulation has not been established in the
following conditions/patient populations:
• Pregnancy
• Pediatric patients (ie, under 22 years of age)
• Nasal or sinus surgery (including history of application of nasal cautery)
or significant trauma
• Severe nasal airway obstruction (eg, severe septal deviation or inferior
turbinate hypertrophy) or vascularized polyp
• Active, severe:
• Systemic allergy
• Chronic seasonal allergies
• Rhinitis or sinusitis requiring treatment such as
antihistamines, decongestants, oral or aerosol steroids
• Untreated nasal infection
• Disabling arthritis, neuropathy, severe dexterity impairment, or limited
motor coordination affecting self-handling of the TrueTear®device
• Use of accessories, transducers, and cables other than those specified or provided
by the manufacturer of this equipment could result in increased electromagnetic
emissions or decreased electromagnetic immunity of this equipment and result in
improper operation. Portable RF communications equipment (including peripherals
such as antenna cables and external antennas) should be used no closer than 30
cm (12 inches) to any part of the TrueTear®device. Otherwise, degradation of the
performance of this equipment could result.
4 PRECAUTIONS
The patient should also be advised of the following (these precautions are also provided in
the patient labeling):
• Before operating the device, the patient should consult their healthcare provider
for instructions.
• If the patient feels pain, discomfort, or numbness in their nose with higher levels
of stimulation or a longer duration of stimulation, they should reduce the level or
the number of times they stimulate the nose. If symptoms persist, they must
discontinue use and contact their provider.
• For proper operation and good hygiene, the disposable tip must be disposed of
every 48 hours and replaced with a new tip.
• Remove any studs, nose rings, or other piercings from the nose prior to using
the device.
• Ophthalmic prescription eye medications (eye drops, gels, or ointments) should not
be used within 30 minutes before or after applying stimulation.
• Nasal sprays should not be used within 30 minutes before or after
applying stimulation.
• Patients with suspected or diagnosed heart disease should follow precautions
recommended by their providers.
• Keep this device out of the reach of children.
• Patients with a severe phobia of placing objects in the nose may not be able to
effectively utilize this device.
• Clean as directed.
• Failure to replace the tip as directed will cause the device to not work properly.
5 POTENTIAL COMPLICATIONS
• Nasal pain, discomfort, or burning sensation
• Transient electrical discomfort
• Nosebleeds
• Nasal congestion
• Excessive sneezing
• Nasal irritation or numbness
• Nasal infection, abrasion, ulceration or inflammation
• Irritation or sensitivity of the target nasal tissue
• Headache, lightheadedness
• Trace blood, dot heme in nostril
• Facial pain or pain around the eye, sinus pain, sore eye
• Increased salivation
• Sensation of teeth vibrating
• Excessive nose running
• Temporary aggravation of symptoms associated with nasal allergies
• Allergic reaction to contact materials
• Permanent nasal scarring with prolonged use
6 TRUETEAR®DEVICE OVERVIEW
The TrueTear®device consists of four distinct parts:
1. A reusable base unit, which produces the electrical stimulation
2. A disposable tip that inserts into the nasal cavity and stimulates the
target intranasal tissue
3. A reusable cover to protect the disposable tip
4. A charger, which recharges the battery inside the base unit
The disposable tip connects to the base unit and contains a hydrogel (similar to the material
used in contact lenses) that provides the contact for conducting the stimulation current, which
is produced by the base unit, to the target site on the inside of the nose. Remove and replace
the disposable tip every 48 hours; a separate cover can be used to protect the disposable tip
between uses. With the disposable tip removed, the base unit can be inverted and placed onto
the charger to replenish the base unit’s battery. The base unit should be recharged every 48
hours or when you change the tip. All images show in this guide are for referencing only.
7 CHARGING THE BATTERY
NOTE: Only use the provided AC adapter for attaching to charger.
1. Ensure the base unit is fully charged if using the device for the first time.
2. If the device has been fully charged and placed on the charger throughout the day
(in between uses), it is not necessary to wait for the LED light to turn from a steady
orange to green.
3. Connect the charger to the wall outlet (120-240V) using the micro USB wall adapter
and cable (Figure 2). CAUTION: The AC adapter provides protection from high
voltages and should only be plugged into easily accessible outlets.
Figure 2. Connecting the charger.
4. Remove the disposable tip from the base unit by rocking the tip away from the buttons—
the disposable tip should disconnect easily. Then place the base unit onto the charger.
An LED light will turn to a steady orange to indicate that the base unit is correctly charging
(Figure 3).
charging charge
complete
page 9 of C-0146 (A) images
charging charge
complete
7a
7b
7c
Figure 3. Placement of base unit on the charger.
hydrogel
Base unit +
disposable tip
Charger
Figure 1. The TrueTear
®
device components.
Cover

5. Remember to charge the base unit every 48 hours. The charging process should take
less than 4 hours to complete. An LED light will turn green to indicate that charging is
complete. The base unit may be removed or left on the charger when charging is
complete (Figure 4).
Figure 4. Upon completion of charge, remove base unit from charger.
Once complete, remove
base unit.
8 ASSEMBLY INSTRUCTIONS
1. Ensure the base unit is fully charged if using the device for the first time (see CHARGING
THE BATTERY).
2. Tear tip pouch at notch to open, and remove disposable tip from the pouch by grasping the
base (as shown in Figure 5). Avoid touching the hydrogel.
Figure 5. Remove the disposable tip from the pouch.
hydrogel
tear at notch to open
Grasp base of disposable
tip to remove from pouch.
3. Connect the disposable tip to the base unit by aligning the tab on the underside of the
disposable tip with the notch on the base unit, then rotate forward until the disposable tip
snaps into place, as shown in Figure 6.
IMPORTANT: DO NOT USE A DISPOSABLE TIP FOR MORE THAN 48 HOURS. The disposable
tip should be replaced every 48 hours. Failure to replace the disposable tip causes the
hydrogel to dry out and may result in ineffective stimulation.
9 STIMULATION INSTRUCTIONS
The following set of instructions is provided to the patient in a separate document; however,
the healthcare provider should confirm the patient’s understanding of these instructions,
including the patient’s demonstration of stimulation and the tearing response, prior to
prescribing the device and, if necessary, at subsequent visits:
1. With the device fully assembled, hold the + button for 5 seconds to turn on the device.
The base unit LED lights will flash to indicate that it has been turned on; the green LED
light will remain lit, as shown in Figure 7.
2. Press the + button to select a desired stimulation intensity level. Blue LED lights show
the level selected.
3. Place thumb near buttons of the base unit, then insert the disposable tip into the nasal
cavity with the buttons pointing towards your lips and face, as shown in Figure 7 above.
4. For effective stimulation, ensure tip is inserted all the way to the top and front of the
nose, as shown in Figure 8.
Rest thumb on the + or —
button. Press + or — to
change levels if desired.
Insert tip into your nose,
as far as is comfortable.
Figure 8.
Target zone for correct insertion of disposable tip
.
5. Gradually increase and adjust stimulation level (using the +/- buttons) until you feel
a gentle tingling in your nose; this feeling is an indication that you are stimulating the
correct tissue location and tears will start forming.
6. There are 5 stimulation intensity levels. The base unit vibrates briefly when a + button
is pressed to indicate an increase or – button is pressed to indicate decrease in
stimulation level. The blue LED light will be lit to indicate the stimulation level selected
(Figure 9).
7. Tip may be repositioned along the inside surface of the nose to achieve the desired
stimulation. At its maximum, the sensation should be mild.
8. If you do not feel any sensation at all, replace the tip with a new tip and try again.
9. If you feel uncomfortable during stimulation, remove the device from your nose.
10. The device automatically turns off after one minute of stimulation. Alternatively, the device
may also be turned off by holding down the - button for 2 seconds. The device will vibrate
and the LED lights will turn off to indicate that the power has been switched off.
11. If you prefer a longer stimulation time, restart the device after it turns off.
12. When finished, clean system with tissue or an alcohol wipe (see CARING FOR DEVICE)
prior to attaching the cover to protect the disposable tip between uses (Figure 10).
Figure 10.
Cover attached to base unit to protect diposable tip.
10 RECOMMENDED STIMULATION SCHEDULE
The patient is to perform intranasal tear stimulation at least twice a day, as needed. For each
instance, stimulation longer than 3 minutes (3 sequential cycles) is not recommended and the
patient should wait for at least 60 minutes before proceeding to the next application.
The device is capable of single-day stimulation up to a limit of 30 minutes, for all stimulation
levels combined. Once the daily limit has been reached, the device will turn on and then off
immediately and will no longer deliver stimulation.
11 CARING FOR THE THE TRUETEAR®DEVICE
The following set of instructions is provided to the patient in a separate document; however,
the healthcare provider should confirm the patient’s understanding of these instructions prior
to prescribing the device and, if necessary, at subsequent visits:
1. Use alcohol wipes to clean the cover, disposable tip, and device between uses.
Avoid damaging the hydrogel.
2. Use alcohol wipes to clean the durable parts of the device including the base, charger, and
cover (including the interior of the cover). Clean the inside of the cover weekly or more
often if needed to ensure proper hygiene.
Figure 11.
Cleaning with alcohol wipes.
3. Do NOT submerge or immerse the base unit, electrical plug, or charger in water or
other liquid.
page 9 of C-0146 (A) images
6a
6b
Figure 12.
Do not rinse base unit or charger in water or any other liquid.
4. Handle with care. Store the TrueTear®device system in a clean, cool, and dry location.
Avoid exposure to extreme temperatures and humidity.
CAUTION: Exposure to direct heat can cause the hydrogel in the disposable tip to dry
out and may result in ineffective stimulation. Avoid touching the metal contacts of
the base unit or charger if either unit is exposed to high temperature extremes
(eg, sitting in a hot car).
page 5 of C-0146 (A) images
3a
Tab
Notch
Device is
“on”
Figure 6. Align the tab to the notch for setup.
The disposable tip only fits one way.
Figure 9. Adjust stimulation by pressing the + or - buttons.
Figure 7. Turning on the device and placing it into the nasal cavity.

12 SUMMARY OF PIVOTAL CLINICAL STUDIES
Two pivotal clinical studies have been conducted with the TrueTear®device. Both studies
evaluated the TrueTear®device’s safety and effectiveness in dry eye patients. Both pivotal
studies (OCUN-009 and OCUN-010) demonstrated the device’s capability to temporarily
increase tear production during stimulation.
Study OCUN-010 demonstrated the device’s capability to improve dry eye symptoms as a
result of stimulation. The next section summarizes both pivotal studies.
Acute Tear Production Pivotal Clinical Trial (OCUN-009)
This pivotal trial, “A Randomized, Controlled, Double-Masked, Multicenter Trial Designed to
Evaluate Acute Tear Production During Neurostimulation With the TrueTear®Device Compared
to Two Control Applications in Patients With Aqueous Deficient Dry Eye,” evaluated the
effectiveness and safety of the TrueTear®device during stimulation.
Potential subjects were required to meet the following main inclusion criteria at screening:
• 22 years of age or older
• Baseline Ocular Surface Disease Index©(OSDI©) score of at least 13 with no
more than three responses of “not applicable”
• In at least one eye, a baseline Jones Schirmer test with anesthetic of ≤ 10 mm/
5 minutes and a cotton swab nasal stimulation Jones Schirmer test at least 7 mm
higher in the same eye
Potential subjects were excluded if they met any of the following criteria:
• Clinically significant corneal epithelial defects at study day (visit 2) prior to
performing the Jones Schirmer tests
• Chronic or recurrent epistaxis, coagulation disorders or conditions
• Nasal or sinus surgery or significant trauma
• Severe nasal airway obstruction or vascularized nasal polyp
• Cardiac demand pacemaker, implanted defibrillator, or other implanted
electronic device
• Disabling arthritis, neuropathy, or limited motor coordination affecting
self-handling of the device
In this 2-visit study, potential subjects underwent a screening (visit 1) to determine eligibility
prior to device use on the study day (visit 2). On the study day, each subject underwent
3 applications, 1 active and 2 control applications, administered in random order. These
applications consisted of the following:
• Active intranasal stimulation (active)
• Active extranasal (off-target) device application (control)
• Sham device intranasal application (control)
The primary effectiveness endpoint was the difference between the Schirmer test score
during active stimulation and during each of the 2 control applications. A crossover linear
model was fit with Schirmer test result as the response variable; sequence, application,
period, and the application by period interaction as fixed effects; and participant (sequence)
as a random effect to account for correlation among observations within a participant.
Pairwise comparisons between the active device and each of the controls were formed using
least-square mean results from the crossover model. The direct clinical benefit of temporarily
increasing tear production as a therapy for patients with dry eye disease was not assessed as
part of this clinical trial.
The primary safety measure was the proportion of subjects reporting 1 or more adverse
events (AEs) in addition to the proportion of subjects reporting device-related AEs. Additional
safety measures included an intranasal speculum examination, slit lamp biomicroscopy,
fluorescein staining, corrected distance visual acuity (CDVA), heart rate (HR), oxygen
saturation (SpO2), blood pressure (BP), and a cardiovascular and pulmonary
symptom assessment.
The study was conducted at 2 sites in the United States and enrolled 48 subjects. The mean
age of the total study population was 56.9 ± 13.2 years. Thirty-nine (81.3%) subjects were
female and 9 (18.8%) were male. The majority (n = 45, 93.8%) of subjects were white, 2
(4.2%) subjects were African-American, and 1 (2.1%) subject was Asian.
The TrueTear®device stimulated a large increase in tear production, and the study met
its primary effectiveness endpoint of increased tear production relative to each of the 2
control applications. An average Schirmer score of 25.3 mm ± 10.7 was observed during
active neurostimulation, compared with only 9.2 mm ± 7.3 for the sham control application
(P< .0001), and 9.5 mm ± 8.2 for the extranasal control application (P< 0.0001)
(Figure 13). The mean difference between Schirmer score with active stimulation versus
sham control application and versus extranasal control application was 16.1 mm and
15.8 mm, respectively.
The TrueTear®device presented an acceptable safety profile in this study, with no serious
adverse events (SAEs) and no AEs that led to discontinuation from the study. Two AEs were
deemed related to or possibly related to the device. These included transient lightheadedness
(asked of patients on the cardiopulmonary questionnaire, and considered possibly related)
and intermittent nose itching (related). Both AEs resolved without sequelae.
Heart rate and BP were slightly increased during stimulation with the neurostimulator device
applied intranasally and returned to prestimulation levels approximately two minutes following
stimulation. Minimal2change was observed in SpO2between the prestimulation, stimulated,
and poststimulation values for the device intranasal or control applications. None of the
changes in vital signs were considered a “dive response” by the masked Clinical Events
Committee, and none were considered device-related AEs. No relevant changes were observed
in intranasal speculum examination, slit lamp biomicroscopy, fluorescein staining, or CDVA.
In conclusion, there was a clinically and statistically significantly higher degree of tear
production during stimulation with the TrueTear®device than with either of the 2 control
applications. Safety during the study was acceptable, and there were no relevant changes in
any cardiopulmonary measures.
Six-Month Pivotal Clinical Trial (OCUN-010)
This pivotal trial, “Single-Arm, Multicenter, Open-Label Study to Evaluate the Safety and
Effectiveness of the TrueTear®device in Subjects With Aqueous Tear Deficient Dry Eye,”
evaluated the safety and effectiveness of the TrueTear®device at multiple time points during
the study (7, 30, 90, and 180 days) for subjects with aqueous tear deficient (ATD) dry eye.
Potential subjects were required to meet the following main inclusion criteria at screening:
• 22 years of age or older
• Baseline OSDI©score of at least 23 with no more than three responses of
“not applicable”
• In at least one eye, a baseline Jones Schirmer test with anesthetic of
≤ 10 mm/5 minutes and a cotton swab nasal stimulation Jones Schirmer test
at least 7 mm higher in the same eye
• Corneal fluorescein staining score of 2 or more in at least one corneal region and a
sum of 4 or more for all corneal regions in the same eye
• No contact lens wear for at least 7 days prior to screening and willingness to forego
contact lens wear for the study duration
Potential subjects were excluded if they met any of the following criteria:
• Change in ophthalmic cyclosporine preparation dosage within 30 days prior to day 0
or anticipated change during study
• Chronic or recurrent epistaxis, coagulation disorders or conditions
• Nasal or sinus surgery or significant trauma
• Cardiac demand pacemaker, implanted defibrillator, or other implanted
electronic device
• Severe nasal airway obstruction or vascularized polyp
• Disabling arthritis, neuropathy, or limited motor coordination affecting self-handling
of the device
Prior to the start of the study, one eye was qualified as the Study eye, and the other eye as
the Qualified Fellow Eye, for which data were also collected to further corroborate device
performance.
Subjects were enrolled at day 0 and were provided with a device for home use. Participants
were instructed to perform intranasal neurostimulation at least 2 times a day and as often as
10 times per day, as needed, and no more than 3 minutes per use. Participants were followed
for 180 days and were seen for follow-up exams at days 7, 30, 90, and 180.
The primary effectiveness measure was the Schirmer test as an assessment of the increase
in acute stimulated tear production in the study eye at day 180 (primary endpoint) and days
0, 7, 30, and 90 (secondary endpoints). Symptoms were assessed with the Ocular Surface
Disease Index [OSDI] at the Screening Visit and days 0, 7 and 30. Analyses were conducted
for the entire eligible population and as well as stratified by dry eye severity subgroup. Dry
eye severity subgroups were determined by the Screening Visit OSDI score where moderate
dry eye was defined as an OSDI total score of 13 to 22 and a severe dry eye was defined
as an OSDI total score of 33 or more. The primary safety assessment was the proportion of
subjects who experienced 1 or more device-related AEs. Additional safety measures included
CDVA, slit lamp biomicroscopy findings, nasal endoscopy, and sensitivity of olfaction (UPSIT)
at study exit compared to baseline.
The primary effectiveness endpoint was the increase in tear production in the study eye
during use of the TrueTear®device compared to the unstimulated tear production as assessed
by the Schirmer test at day 180. Secondary effectiveness endpoints were the increase in tear
production in the study eye during use of the device at the other study visits. The analysis
used a paired t test or Wilcoxon signed-rank test, as appropriate, and was evaluated at a
one-sided αof 0.025. Symptoms were assessed by analyses of the mean OSDI change from
baseline and proportion of subjects that improved or worsened in symptoms by a clinically
important difference as measured with OSDI. The minimal clinically important difference
(MCID) thresholds for the analyses were based on those characterized by Miller et al (Arch
Ophthalmol. 2010;128(1):94-101). Safety was assessed by an analysis of adverse events
in addition to several specific safety measures, including olfaction sensitivity as measured
using the UPSIT, nasal endoscopic exam, assessment of corneal edema, CDVA, and slit lamp
biomicroscopy.
Ninety-seven adult subjects were enrolled at 3 sites in the United States, and 89 subjects
were followed to day 180. The mean age of the total study population was 61.1 ± 10.0 years.
Seventy-seven (79.4%) subjects were female and 20 (20.6%) subjects were male. Seventy-
eight subjects (80.4 %) were white, 16 (16.5%) subjects were African-American, and 3 (3.1%)
subjects were Asian. Eight of the subjects (8.3%) were Hispanic or Latino.
Subject accountability is shown in Table 1.
Table 1: Subject accountability
Enrolled = 97
Day 0 Day 7 Day 30 Day 90 Day 180
Available for
analysis 97 (100%) 95 (98%) 91 (94%) 89 (92%) 89 (92%)
Missing 0 0 2 (2%) 0 0
Discontinued 0 2 (2%) 6 (6%) 8 (8%) 8 (8%)
Subject choice 0 1 (1%) 3 (3%) 4 (4%) 4 (4%)
Adverse event 0 0 0 3 (3%) 3 (3%)
Other 0 1 (1%) 1 (1%) 1 (1%) 1 (1%)
Percentages are based on the total number of subjects enrolled.
The study met its primary effectiveness endpoint and each of its secondary effectiveness
endpoints. Mean acute stimulated tear production in the study eye was statistically
significantly better than the mean unstimulated tear production on day 180 (P< .0001,
one-sided paired ttest). In comparing the stimulated vs unstimulated tear production during
the study, following the initial stimulation, there was a trend toward decreased effectiveness
(tear production) with time with the use of the TrueTear®device; this trend appeared to
plateau toward the end of the study. The mechanism for this decrease has not been identified
and was not analyzed as part of this study. The mean difference in Schirmer score (stimulated
versus unstimulated) was 18.0 mm on day 0, 13.1 mm on day 7, 8.1 mm on day 30, 8.3 mm on
day 90, and 9.4 mm on day 180.
Figure 13.
Schirmer test scores of study eye by device application group.
40.0
35.0
30.0
25.0
20.0
15.0
10.0
5.0
0.0
Schirmer Scores – Study Eye
Intranasal
ªP < .0001
ª
ª
ExtranasalSham
Application
Schirmer Score (mm)

Statistical significance was also seen at day 180 for the qualified fellow eye. The mean (SD)
difference between stimulated and unstimulated tear production at day 180 was 9.4 mm (10.9)
and 10.2 mm (9.9) for the study eye and qualified fellow eye, respectively (Table 2).
Table 2: Acute tear production at day 180
The primary study endpoint outcomes at day 180 were stratified by age, sex, race, and
baseline Schirmer score. The outcomes were statistically significant for all age strata except
those subjects over age 70, which was composed of only 16 subjects. The results were also
statistically significant for both males and females, as well as white and nonwhite races.
Subjects with a baseline Schirmer score of 0 to 5 mm experienced a mean (SD) increase in
stimulated Schirmer score of 8.9 (11.4) mm, and subjects with a baseline Schirmer score
of 6 to 10 mm experienced a mean increase of 9.8 (10.5) mm. The results were statistically
significant for both the 0- to 5-mm group and the 6- to 10-mm group.
Secondary effectiveness endpoints included the acute stimulated tear production in the
study eye on days 0, 7, 30, and 90. Mean acute stimulated tear production in the study eye
following device application was statistically significantly better than the mean unstimulated
tear production on days 0, 7, 30, and 90 overall (Table 3). Overall, mean (SD) differences in tear
production in the study eye compared to baseline ranged from 8.1 mm (11.2) to 18.0 mm (9.6)
at the 5 study time points.
Table 3: Acute tear production in the study eye by visit.
Table 3: Acute tear production in the study eye by visit.(Continued)
Tear production at each follow-up visit including 180 days (6 months) is shown in Figure 14.
Symptom assessment was based on the 12-item OSDI questionnaire at Screening, day 0, day 7,
and day 30. The OSDI uses a 5-unit scale (0 = none of the time, 4 = all of the time) for question
responses. Subjects were stratified into moderate and severe dry eye subgroups based on
Screening Visit OSDI total score. The proportion of subjects with a clinically important change
in OSDI at follow-up days 7 and 30 for all available subjects stratified by dry eye severity
subgroup and by the upper and lower limit of the MCID was analyzed. Of the 97 subjects
that were enrolled, 77 had severe dry eye symptoms at the start of the study and were seen
following treatment. Of these subjects, between 18 (23%) and 33 (43%) were shown to have a
clinically meaningful improvement in their symptoms (Table 4). There were more subjects with
severe dry eye symptoms that had a meaningful improvement in symptoms from baseline as
measured with the OSDI than the number with meaningful worsening of symptoms at day 7 and
at day 30. The sample size of the moderate dry eye group was too small to make meaningful
inferences regarding the results.
Table 4: Proportion of Subjects With Severe Dry Eye Symptoms at Screening
with Clinically Important Change in the OSDI* From Baseline at Days 7 and 30.
The safety profile of the TrueTear
®
device was acceptable in this study, with no
device-related SAEs, and only mild device-related AEs that were largely nasal in
nature (Table 4). All device-related AEs (mostly mild discomfort or epistaxis) were
evident to the patients and therefore self-limiting (with the exception of one case of
chapped skin around the nostrils that resolved with over-the-counter Neosporin®)
since patients could remove the device and discontinue stimulation at any time. The
incidence of device-related AEs decreased over the course of the study, with the
highest number (22, 61%) occurring in the first month, followed by 6 (17%) mild AEs
that occurred between days 31 and 90, and 8 (22%) mild AEs occurring in the final 3
months of the study. These 36 device-related mild AEs occurred in 97 subjects with
27,338 cumulative stimulations.
Table 5: Proportion of subjects experiencing adverse event–related or
possibly related to the TrueTear
®
device–safety population
No relevant changes were observed in olfaction, endoscopic exam, corneal edema, CDVA,
or slit lamp findings over the 180-day study period. Seven serious adverse events were
reported; however, none of these events were device related, and all were nonocular and
nonnasal in nature.
All Subjects
(N = 97)
Stimulated
Schirmer Test Unstimulated
Schirmer Test
Study Eye
n 89 89
Mean (SD) 17.28 (11.948) 7.92 (6.386)
Median 13.00 6.00
Min-Max 0.0, 35.0 0.0, 28.0
Mean Difference (SD), Stimulated vs Unstimulated 9.36 (10.902) ---
95% CI for the Mean Difference (7.06, 11.66) ---
Pvalue, paired ttest < .0001 ---
Pvalue, Wilcoxon signed-rank test < .0001 ---
Qualied Fellow Eye
n 40 40
Mean (SD) 16.73 (11.071) 6.55 (5.514)
Median 14.00 5.00
Min-Max 0.0, 35.0 0.0, 23.0
Mean Difference (SD), Stimulated vs Unstimulated 10.18 (9.884) ---
95% CI for the Mean Difference (7.01, 13.34) ---
Pvalue, paired ttest < .0001 ---
Pvalue, Wilcoxon signed-rank test < .0001 ---
Abbreviations: CI: condence intervals; Min: minimum; Max: maximum; N: total number of
subjects; n: number of subjects in given subgroup; SD: standard deviation.
All Subjects
(N = 97)
Stimulated
Schirmer Test Unstimulated
Schirmer Test
Day 0 (Baseline)
n 97 97
Mean (SD) 26.20 (10.583) 8.19 (6.621)
Median 33.00 7.00
Min-Max 3.0, 35.0 0.0, 30.0
Mean Difference (SD), Stimulated vs Unstimulated 18.01 (9.588) ---
95% CI for the Mean Difference (16.08, 19.94) ---
Pvalue, paired ttest < .0001 ---
Pvalue, Wilcoxon signed-rank test < .0001 ---
Day 7
n 95 95
Mean (SD) 19.73 (11.142) 6.63 (6.316)
Median 19.00 5.00
Min-Max 2.0, 35.0 0.0, 33.0
Mean Difference (SD), Stimulated vs Unstimulated 13.09 (9.702) ---
95% CI for the Mean Difference (11.12, 15.07) ---
Pvalue, paired ttest < .0001 ---
Pvalue, Wilcoxon signed-rank test < .0001 ---
Day 30
n 91 91
Mean (SD) 17.40 (10.742) 9.34 (6.665)
Median 14.00 9.00
Min-Max 1.0, 35.0 0.0, 34.0
Mean Difference (SD), Stimulated vs Unstimulated 8.05 (11.150) ---
95% CI for the Mean Difference (5.73, 10.38) ---
Pvalue, paired ttest < .0001 ---
Pvalue, Wilcoxon signed-rank test < .0001 ---
Day 90
n 89 89
Mean (SD) 16.22 (11.206) 7.92 (6.567)
Median 12.00 6.00
Min-Max 2.0, 35.0 0.0, 26.0
Mean Difference (SD), Stimulated vs Unstimulated 8.26 (10.437) ---
95% CI for the Mean Difference (6.06, 10.46) ---
Pvalue, paired ttest < .0001 ---
Pvalue, Wilcoxon signed-rank test < .0001 ---
Day 180
n 89 89
Mean (SD) 17.28 (11.948) 7.92 (6.386)
Median 13.00 6.00
Min-Max 0.0, 35.0 0.0, 28.0
Mean Difference (SD), Stimulated vs Unstimulated 9.36 (10.902) ---
95% CI for the Mean Difference (7.06, 11.66) ---
Pvalue, paired ttest < .0001 ---
Pvalue, Wilcoxon signed-rank test < .0001 ---
Abbreviations: CI: condence intervals; Min: minimum; Max: maximum; N: total number of
subjects; n: number of subjects in given subgroup; SD: standard deviation.
All Subjects
(N = 97)
Stimulated
Schirmer Test Unstimulated
Schirmer Test
Day 0 (Baseline)
n 97 97
Mean (SD) 26.20 (10.583) 8.19 (6.621)
Median 33.00 7.00
Min-Max 3.0, 35.0 0.0, 30.0
Mean Difference (SD), Stimulated vs Unstimulated 18.01 (9.588) ---
95% CI for the Mean Difference (16.08, 19.94) ---
Pvalue, paired ttest < .0001 ---
Pvalue, Wilcoxon signed-rank test < .0001 ---
Day 7
n 95 95
Mean (SD) 19.73 (11.142) 6.63 (6.316)
Median 19.00 5.00
Min-Max 2.0, 35.0 0.0, 33.0
Mean Difference (SD), Stimulated vs Unstimulated 13.09 (9.702) ---
95% CI for the Mean Difference (11.12, 15.07) ---
Pvalue, paired ttest < .0001 ---
Pvalue, Wilcoxon signed-rank test < .0001 ---
Day 30
n 91 91
Mean (SD) 17.40 (10.742) 9.34 (6.665)
Median 14.00 9.00
Min-Max 1.0, 35.0 0.0, 34.0
Mean Difference (SD), Stimulated vs Unstimulated 8.05 (11.150) ---
95% CI for the Mean Difference (5.73, 10.38) ---
Pvalue, paired ttest < .0001 ---
Pvalue, Wilcoxon signed-rank test < .0001 ---
Day 90
n 89 89
Mean (SD) 16.22 (11.206) 7.92 (6.567)
Median 12.00 6.00
Min-Max 2.0, 35.0 0.0, 26.0
Mean Difference (SD), Stimulated vs Unstimulated 8.26 (10.437) ---
95% CI for the Mean Difference (6.06, 10.46) ---
Pvalue, paired ttest < .0001 ---
Pvalue, Wilcoxon signed-rank test < .0001 ---
Day 180
n 89 89
Mean (SD) 17.28 (11.948) 7.92 (6.386)
Median 13.00 6.00
Min-Max 0.0, 35.0 0.0, 28.0
Mean Difference (SD), Stimulated vs Unstimulated 9.36 (10.902) ---
95% CI for the Mean Difference (7.06, 11.66) ---
Pvalue, paired ttest < .0001 ---
Pvalue, Wilcoxon signed-rank test < .0001 ---
Abbreviations: CI: condence intervals; Min: minimum; Max: maximum; N: total number of
subjects; n: number of subjects in given subgroup; SD: standard deviation.
All Subjects
(N = 97)
Stimulated
Schirmer Test Unstimulated
Schirmer Test
Day 0 (Baseline)
n 97 97
Mean (SD) 26.20 (10.583) 8.19 (6.621)
Median 33.00 7.00
Min-Max 3.0, 35.0 0.0, 30.0
Mean Difference (SD), Stimulated vs Unstimulated 18.01 (9.588) ---
95% CI for the Mean Difference (16.08, 19.94) ---
Pvalue, paired ttest < .0001 ---
Pvalue, Wilcoxon signed-rank test < .0001 ---
Day 7
n 95 95
Mean (SD) 19.73 (11.142) 6.63 (6.316)
Median 19.00 5.00
Min-Max 2.0, 35.0 0.0, 33.0
Mean Difference (SD), Stimulated vs Unstimulated 13.09 (9.702) ---
95% CI for the Mean Difference (11.12, 15.07) ---
Pvalue, paired ttest < .0001 ---
Pvalue, Wilcoxon signed-rank test < .0001 ---
Day 30
n 91 91
Mean (SD) 17.40 (10.742) 9.34 (6.665)
Median 14.00 9.00
Min-Max 1.0, 35.0 0.0, 34.0
Mean Difference (SD), Stimulated vs Unstimulated 8.05 (11.150) ---
95% CI for the Mean Difference (5.73, 10.38) ---
Pvalue, paired ttest < .0001 ---
Pvalue, Wilcoxon signed-rank test < .0001 ---
Day 90
n 89 89
Mean (SD) 16.22 (11.206) 7.92 (6.567)
Median 12.00 6.00
Min-Max 2.0, 35.0 0.0, 26.0
Mean Difference (SD), Stimulated vs Unstimulated 8.26 (10.437) ---
95% CI for the Mean Difference (6.06, 10.46) ---
Pvalue, paired ttest < .0001 ---
Pvalue, Wilcoxon signed-rank test < .0001 ---
Day 180
n 89 89
Mean (SD) 17.28 (11.948) 7.92 (6.386)
Median 13.00 6.00
Min-Max 0.0, 35.0 0.0, 28.0
Mean Difference (SD), Stimulated vs Unstimulated 9.36 (10.902) ---
95% CI for the Mean Difference (7.06, 11.66) ---
Pvalue, paired ttest < .0001 ---
Pvalue, Wilcoxon signed-rank test < .0001 ---
Abbreviations: CI: condence intervals; Min: minimum; Max: maximum; N: total number of
subjects; n: number of subjects in given subgroup; SD: standard deviation.
Figure 14: Acute tear production, study eye.
30
25
20
15
10
5
0
Day 7
Day 30
Day 90
Day 180
Baseline
Visit
Unstimulated MeanStimulated Mean
Mean Schirmer Test Result (mm)
Cohort MCID** Change Day 7 Day 30
Severe Dry Eye Subgroup
7.3 Improved 42.86% (33/77) 38.67% (29/75)
Worsened 12.99% (10/77) 12.00% (9/75)
13.4 Improved 23.38% (18/77) 25.33% (19/75)
Worsened 5.19% (4/77) 6.67% (5/75)
*OSDI: Ocular Surface Disease Index
** MCID: Minimal Clinically Important Difference
Adverse Event Description Number of Subjects
(N = 97) Percentage
Nasal pain, discomfort, or burning 10 10.3%
Transient electrical discomfort 5 5.2%
Nosebleed 5 5.2%
Nasal congestion 3 3.1%
Headaches 2 2.1%
Trace blood, dot heme in nostril 2 2.1%
Facial pain 2 2.1%
Sore eye 1 1.0%
Sinus pain 1 1.0%
Periorbital pain 1 1.0%
Runny nose 1 1.0%
Nasal ulcers 1 1.0%
Lightheadedness 1 1.0%
Total Subjects 30*30.9%
*Some subjects had more than one adverse event.

The device was applied for an average of 1.7±1.5 times per day with an average daily
application time of 130±159 seconds/day (2.16±2.66 minutes/day). Subjects applied the
device a total of 27,338 times during the study, and the total device application time for the
study was 34,726 minutes. The majority of application time was at Level 2 (≈ 37%), Level 3
(≈ 37%), and Level 4 (≈ 19%), with less application time at Level 1 (≈ 3%) and Level 5 (≈ 5%).
The circuitry within the device adjusts the voltage, up to a maximum of 13V, in order to achieve
the consistent peak current level. As the impedance rises above the maximum value, less
than the targeted peak current will be provided. Table 5 also shows, for each user-selected
stimulation level, the percentage of impedance measurements in the OCUN-010 trial that were
less than or equal to the maximum load impedance, and reflects the proportion of applications
that resulted in full peak current delivery.
Table 6: Impedance summary, OCUN-010 study
Level Peak Current
(mA)
Maximum Impedance for Full Peak
Current Delivery (kOhms)
% of Impedance Measurements Less Than
Maximum for Each Level
1 0.7 18.6 100.0%
(48,180/48,180)
2 1.5 8.7 96.2%
(450,223/468,209)
3 2.5 5.2 82.7%
(327,092/395,508)
4 3.7 3.5 76.4%
(158,221/206,976)
5 5.0 2.6 66.9%
(32,322/48,304)
All 87.1%
(1,016,038/1,167,177)
The mean number of device applications per subject over the study period was 288
(SD: 154 applications, range: 12-685). The mean duration of the TrueTear®device use per
subject was 21,932 seconds or 365.5 minutes (SD: 18,582 seconds, range: 1,745-128,659).
In conclusion, a clinically and statistically significant increase in tear production during
stimulation in the study eye at day 180 and all other visits was observed. The device also
exhibited an acceptable safety profile, with no device-related SAEs and a decrease over time
in the incidence of AEs, largely mild and self-limiting, for subjects with 27,338 cumulative
stimulation events.
13 COMPLAINT REPORTING
If your patient reports a problem with the device, please contact the manufacturer at
1-866-502-8327.
14 ELECTRICAL SPECIFICATIONS
14.1 ELECTROMAGNETIC COMPATIBILITY
The TrueTear®device has been tested for immunity to electrostatic discharge, radio frequency
interference, proximity RF fields from wireless equipment, and power frequency magnetic
fields, as specified in the tables below. Emissions of energy are not likely to cause
interference with nearby electrical equipment.
Guidance and Manufacturer’s Declaration – Emissions
Medical Equipment and Medical Systems
The TrueTear® device is intended for use in the electromagnetic environment specied
below. The customer or user of the TrueTear®device should ensure that it is used in
such an environment.
Emissions Test Compliance Electromagnetic Environment – Guidance
RF Emissions
CISPR 11 Group 1
The TrueTear®device uses RF energy only
for its internal function. Therefore, its RF
emissions are very low and are not likely to
cause any interference in nearby electronic
equipment.
RF Emissions Class B
The TrueTear®device is suitable for use in
all establishments, including domestic
establishments and those directly
connected to the public low-voltage power
supply network that supplies buildings used
for domestic purposes.
Harmonics
EN 61000-3-2 Class A
Flicker
EN 61000-3-3 Complies
Guidance and Manufacturer’s Declaration – Emissions
Medical Equipment and Medical Systems
The TrueTear® device contains a fully certied Bluetooth®transmitter module. This device
complies with Part 15 of the FCC Rules. Operation of the Bluetooth transceiver is subject
to the following two conditions: (1) this device may not cause harmful interference, and (2)
this device must accept any interference received.
Specication Description
Standard Bluetooth 4.1
ISM Frequency Band 2.4 ~ 2.48 GHz
Channels 0-39
Transmit Power +7.5 dBm
Modulation Method GFSK
Max Data Rate 1 Mbps
30-60 Hz
Guidance and Manufacturer’s Declaration – Immunity
Medical Equipment and Medical Systems
The TrueTear®device is intended for use in the electromagnetic environment
specied below. The customer or user of the TrueTear®device should ensure that
it is used in such an environment.
Immunity Test IEC 60601 Test
Level Compliance Level Electromagnetic Environment –
Guidance
ESD
IEC 61000-4-2
±8kV Contact
±15kV Air
±8kV Contact
±15kV Air
Floors should be wood, concrete
or ceramic tile. If floors are
synthetic, the r/h should be at
least 30%.
EFT
IEC 61000-4-4
±2kV Mains
±1kV I/Os
±2kV Mains
±1kV I/Os
Mains power quality should be
that of a typical commercial or
hospital environment.
Surge
IEC 61000-4-5
±1kV Differential
±2kV Common
±1kV Differential
±2kV Common
Mains power quality should be
that of a typical commercial or
hospital environment.
Voltage Dips/
Dropout
IEC 61000-4-11
>95% Dip for
0.5 Cycle
>95% Dip for
1 Cycle
30% Dip for
25/30 Cycles
>95% Dip for
250/300 Cycles
>95% Dip for
0.5 Cycle
>95% Dip for
1 Cycle
30% Dip for
25/30 Cycles
>95% Dip for
250/300 Cycles
Mains power quality should be
that of a typical commercial or
hospital environment. If the user
of the TrueTear®device requires
continued operation during
power mains interruptions,
it is recommended that the
TrueTear®device be powered
from an uninterruptible power
supply or battery.
Power
Frequency
50/60Hz
Magnetic Field
IEC 61000-4-8
30A/m 30A/m
Power frequency magnetic
elds should be that of a
typical commercial or hospital
environment.
Conducted RF
IEC 61000-4-6
3 V
0.15 MHz-80 MHz
6 V in ISM and
amateur radio
bands between
0.15 MHz and 80
MHz
80 % AM at 1 kHz
3 V
0.15 MHz-80 MHz
6 V in ISM and
amateur radio
bands between
0.15 MHz and 80
MHz
80 % AM at 1 kHz
Home Healthcare Environment
Radiated RF
IEC 61000-4-3
10 V/m
80 MHz – 2.7 GHz
80 % AM at 1 kHz
10 V/m
80 MHz – 2.7 GHz
80 % AM at 1 kHz
Home Healthcare Environment

15 EXPECTED SERVICE LIFE
Base unit, charger: 3 years from date of original purchase.
Tip assemblies: expiration date provided on product labeling.
16 DISPOSAL & REPLACEMENT
The base unit, charger, and AC adapter should be returned to the local distributor for recycling
and disposal in accordance with any applicable local, state, and national regulations for
disposal of electronic equipment.
Tip assemblies may be discarded with regular trash. The patient is instructed to contact
their doctor if any portion of the system is not operating properly or if they need additional
supplies.
17 Bluetooth®
This device includes Bluetooth®Smart wireless technology. This feature allows patients
to download their TrueTear®device data so they can view and track their usage on their
smartphone via the TrueTear®mobile app. The Bluetooth®feature does not have to be on
for patients to use the TrueTear®device. For more information on using Bluetooth ®and the
TrueTear®mobile app, please visit www.truetear.com/app.
The Bluetooth®word mark and logos are registered trademarks owned by Bluetooth SIG, Inc.
and any use of such marks by Allergan is under license. Other trademarks and trade names
are those of respective owners.
18 FCC COMPLIANCE
This device contains FCC ID: T9JRN4020. This device complies with Part 15 of the FCC Rules.
Operation is subject to the following two conditions: (1) this device may not cause harmful
interference, and (2) this device must accept any interference received, including interference
that may cause undesired operation.
This equipment has been tested and found to comply with the limits for a Class B digital
device, pursuant to part 15 of the FCC Rules. These limits are designed to provide reasonable
protection against harmful interference in a residential installation. This equipment generates,
uses and can radiate radio frequency energy, and if not installed and used in accordance with
the instructions, may cause harmful interference to radio communications. However, there
is no guarantee that interference will not occur in a particular installation. If this equipment
does cause harmful interference to radio or television reception, which can be determined by
turning the equipment off and on, the user is encouraged to try to correct the interference by
one or more of the following measures:
• Reorient or relocate the receiving antenna
• Increase the separation between the equipment and receiver
• Connect the equipment into an outlet on a circuit different from that to which the
receiver is connected
Consult the dealer or an experienced radio/TV technician for help.
19 ENVIRONMENTAL OPERATING CONDITIONS
Ambient temperature range: 5°C to 40°C
Relative humidity range: 20% to 90%
20 SYMBOLS & MARKINGS
ALLERGAN
4410 Rosewood Lane
Pleasanton, CA 94588
USA
1-866-502-TEAR (8327)
www.truetear.com
© 2018 Allergan.All rights reserved. All trademarks are the property of their respective owners.
Allergan.com C-0481 Revision A (July 2018)
Guidance and Manufacturer’s Declaration –
Immunity to RF wireless communications equipment
ME Equipment and ME Systems
The TrueTear®device is intended for use in the electromagnetic environment
specied below. The customer or user of the TrueTear®device should ensure that
it is used in such an environment.
Test Band¹
Service¹ Modulation²
Maximum
Power Distance Immunity
Test Level
MHz MHz W Meters (V/m)
385 380 -
390 TETRA 400 Pulse modulation²
18 Hz 1.8 0.3 27
450 430 -
470
GMRS 460,
FRS 460
FM³ ± 5 kHz
deviation 1 kHz sine 2 0.3 28
710
745
780
704 -
787
LTE Band
13, 17
Pulse
modulation² 217 Hz 0.2 0.3 9
810
870
930
800 -
960
GSM
800/900,
TETRA 800,
iDEN 820,
CDMA 850,
LTE Band 5
Pulse
modulation² 18 Hz 2 0.3 28
1720
1845
1970
1700 -
1900
GSM 1800;
CDMA 1900;
GSM 1900;
DECT; LTE
Band 1, 3, 4,
25; UMTS
Pulse
modulation² 217 Hz 2 0.3 28
2450 2400 -
2570
Bluetooth,
WLAN,
802.11 b/g/n,
RFID 2450,
LTE Band 7
Pulse modulation²
217 Hz 2 0.3 28
5240
5500
5785
5100 -
5800
WLAN
802.11a/n
Pulse modulation²
217 Hz 0.2 0.3 9
NOTE: If necessary to achieve the IMMUNITY TEST LEVEL, the distance between the
transmitting antenna and the ME EQUIPMENT or ME SYSTEM may be reduced to 1 m.
The 1 m test distance is permitted by IEC 61000-4-3.
¹ For some services, only the uplink frequencies are included.
² The carrier shall be modulated using a 50% duty cycle square wave signal.
³ As an alternative to FM modulation, 50% pulse modulation at 18 Hz may be used
because while it does not represent actual modulation, it would be worst case.
Bluetooth®
Other manuals for TrueTear
2
Table of contents
Other Allergan Medical Equipment manuals
Popular Medical Equipment manuals by other brands

Getinge
Getinge Arjohuntleigh Nimbus 3 Professional Instructions for use

Mettler Electronics
Mettler Electronics Sonicator 730 Maintenance manual

Pressalit Care
Pressalit Care R1100 Mounting instruction

Denas MS
Denas MS DENAS-T operating manual

bort medical
bort medical ActiveColor quick guide

AccuVein
AccuVein AV400 user manual