1 Introduction
LMT 68651c 02/2022
EN | 3
1 Introduction
1.1
Intended use
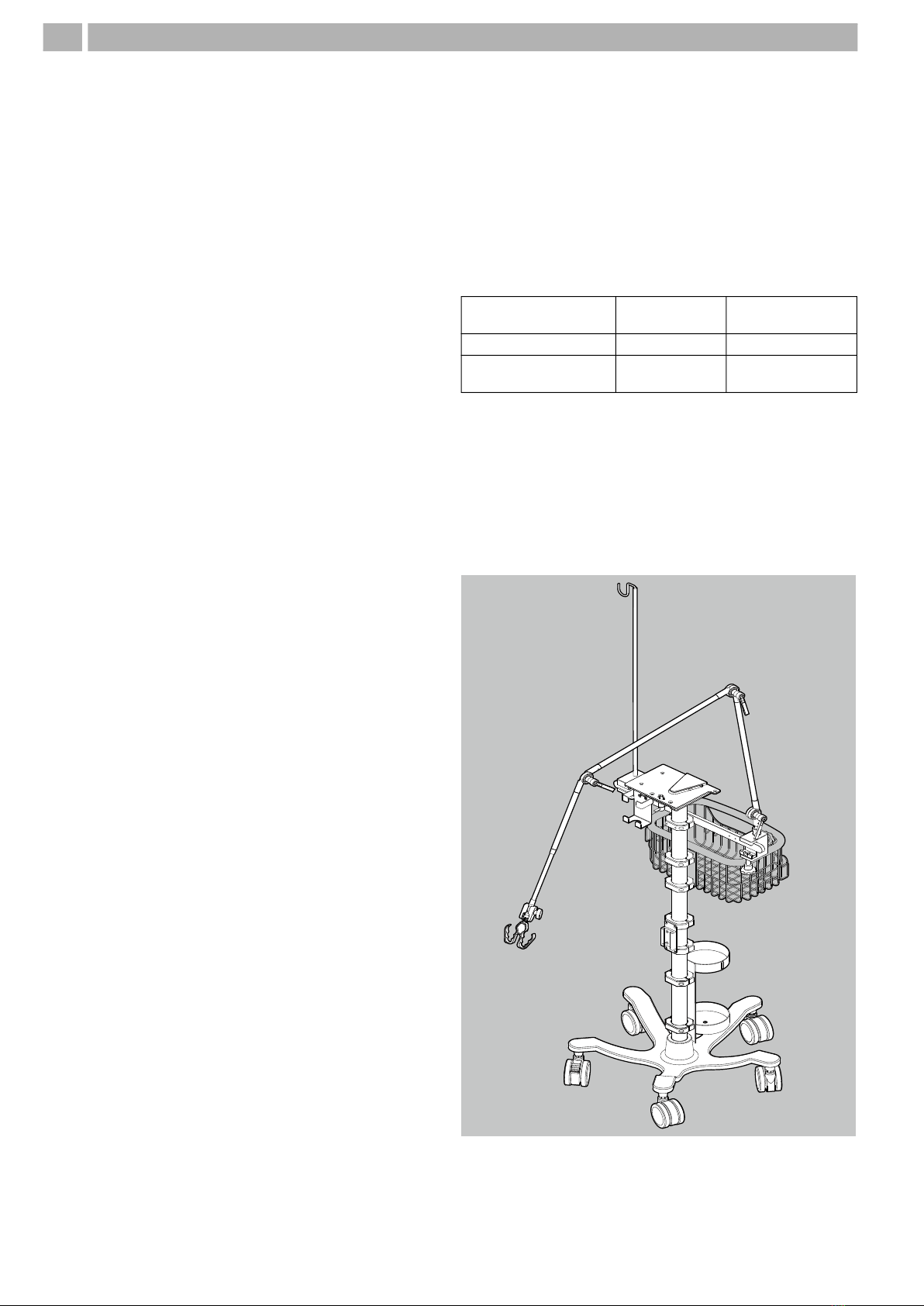
The LM150TD LUISA ventilator is for the life-support and
non-life-support ventilation of patients who require
mechanical ventilation. It can be used for pediatric or adult
patients with a minimum tidal volume of 30 ml.
The LM150TD is suitable for use in the domestic
environment, in care facilities, and in hospitals, as well as for
mobile applications, for example in a wheelchair or on a
transport gurney. It can be used for invasive and non-invasive
ventilation.
Non-specialist users with adequate training and specialist
users can operate the device.
1.2
Description of function
The device can be used with both invasive and non-invasive
patient/ventilator interfaces. The leakage circuit can also be
used invasively.
A blower takes in ambient air through a filter and pumps it
through the ventilation tube and the patient/ventilator
interface to the patient. The blower is controlled to suit
respiratory phases on the basis of the signals detected by the
pressure and flow sensors.
The user interface is for displaying and setting the available
parameters and alarms.
The device can be used with a leakage circuit, with a single
circuit with valve or with a double circuit. With the leakage
circuit, the exhaled air containing CO2 is continuously
flushed out via an exhalation system. With a single circuit
with valve and with a double circuit, the patient’s exhalation
is controlled by a valve.
In High Flow mode (HFT mode), the device pumps the set
flow to an external humidifier suitable for HFT. This
conditions the respiratory gas in terms of temperature and
humidity. The patient connection is made using accessories
suitable for HFT. HFT mode (if available) and MPV mode are
not respiration support modes within the meaning of
standard ISO 80601-2-72. As no permanent and/or sealed
connection is made between the corresponding interfaces
and the patient’s airway, some specifications such as
disconnection detection do not apply.
Oxygen can be supplied via the oxygen inlet.
If required, the FiO2 concentration delivered by the device
can be measured using an integrated FiO2 cell. External SpO2
measurement can also be connected.
The power is supplied by an external power supply unit.
The device has an integrated battery, so it can continue to be
operated without interruption in the event of a power
outage. In addition, a maximum of two external batteries
can be connected to operate the device.
Therapy data are stored in the device and can additionally be
loaded on a USB-C flash drive and analyzed by PC software.
1.3
User qualification
The person operating the device is referred to in these
instructions for use as the user. All users must receive
training or instruction on how to operate the device.
A distinction is drawn between specialist users (experts) and
non-specialist users. The following groups of people make
up both groups:
.
PERSON DESCRIPTION USER QUALIFICATION
Patient Person receiving the therapy Persons with no specialist medical or nursing knowledge.
Following an introduction by the medical professional on
how the device works and how to use it, these
individuals are regarded as non-specialist users.
Non-specialist
user Patient, relative and other caregivers
Owner/operator
Health care facility responsible for ensuring the
compatibility of the device and of all the
components or accessories associated with the
patient before use (e.g., a hospital).
Following training by the manufacturer or by a specialist
expressly authorized by the manufacturer on how the
device works and how to use it, these individuals are
regarded as specialist users.
Medical
professional
Person with state-approved qualification in a
medical profession (e.g., physician, respiratory
therapist, medical technician)
Following training by the manufacturer or trained
owner/operator on how the device works and how to
use it, the persons with specialist knowledge of the
therapy and device (e.g., medical specialists, nursing
specialists, service specialist) are regarded as specialist
users.
Nursing
specialist
Person with state-approved qualification in a
nursing profession
Specialist dealer
Person or organization that markets, but does
not itself manufacture a product. The specialist
dealer can also provide a support function.
Following training by the manufacturer on how the
device works and how to use it, these individuals are
regarded as specialist users.