balanSys REV – Extension Gap First: 3in1 – 9
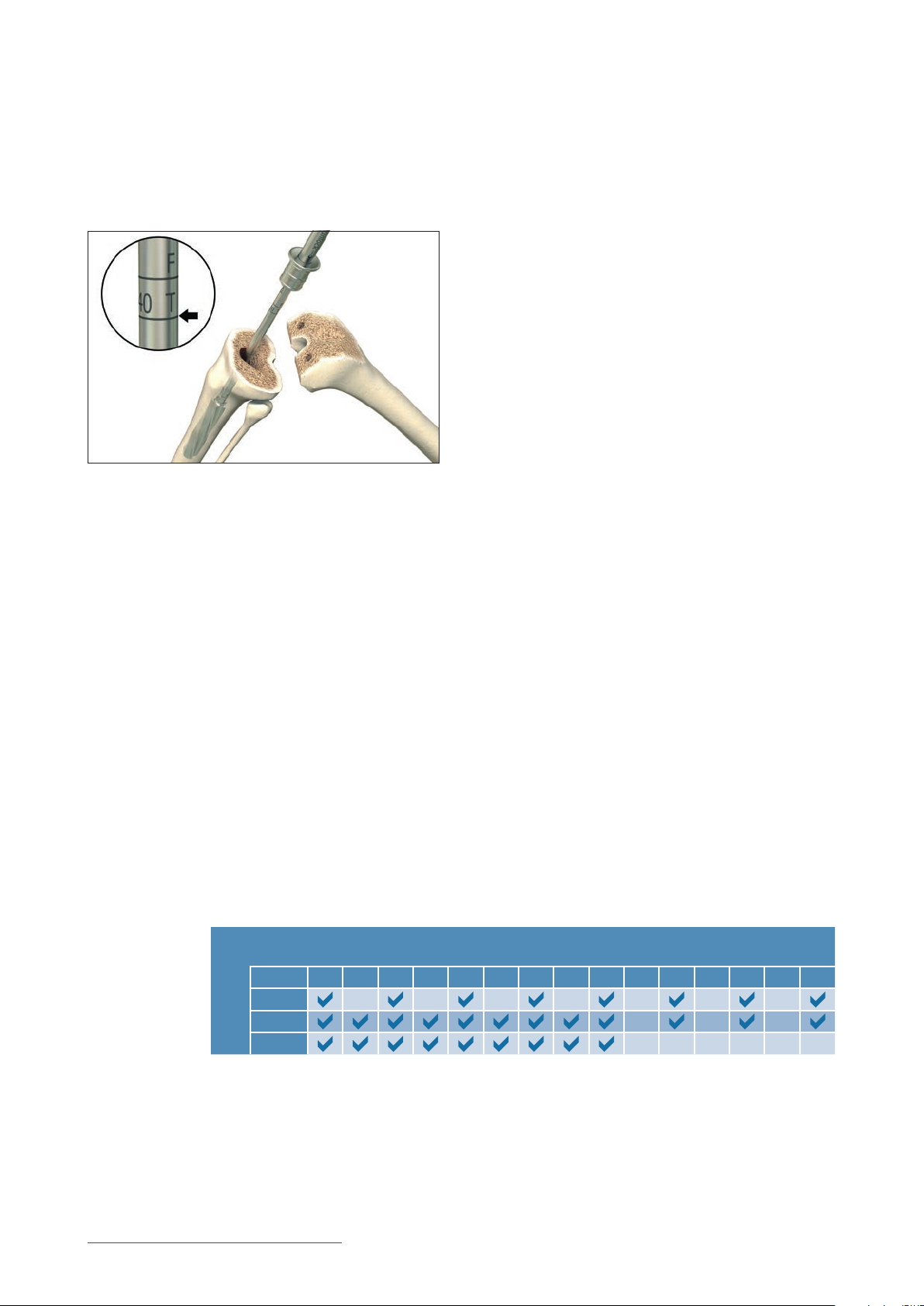
Extraction of primary components
After adequate exposure of all components has been achieved, attention is turned
to component removal. If known, the manufacturer of the components to be re-
moved should be referred for explantation. Usually, the removal of the components is
achieved through dissection of the interface between the prosthesis and the cement
or at the prosthetic/ bone interface. Most surgeons prefer to remove the femoral
component first in order to improve visualization of the posterior tibial component.
A thin, flexible osteotome or a thin oscillating or reciprocating saw should be used
to cut the prosthetic interface in order to allow removal with minimal bone loss.
Angled osteotomes can be helpful in loosening and freeing the condylar portions of
the femoral components. Providing the interfaces have been adequately freed, only
minimal force will be required to remove the femoral component. Removal of the
tibial component is then carried out in a similar fashion. As bone cement fails most
easily in tension, a controlled, well-placed blow will generally dislodge the tibial
component.
Excessive force to remove the components can lead to
femoral fracture or extensive bone loss.
In case the patella was resurfaced previously with a balanSys Patella, special atten-
tion should be given to the patella implant: if the patella implant is securely fixed,
well-positioned and does not show excessive wear then it may be left and protected
for the remainder of the case. If the patellar implant should be revised, removal is
most easily performed with an oscillating saw at the cement interface. Residual
cement and polyethylene plugs from the component may then be removed with a
small, high-speed burr. Great care must be taken during this stage of the procedure
in order to ensure that adequate patellar bone stock remains for revision component
placement so that fracture is prevented.
Once components have been removed, the remaining cement must be removed
with curettes, cement osteotomes or other appropriate instruments. The wounds
can be irrigated pulse lavage to remove loose debris and attention can then be
turned to the reconstructive portion of the procedure.
In cases you prefer retaining a stable balanSys BICONDYLAR component,
make sure to protect all articulation surfaces against damage.
Any wear, scratch or mark on an articulating implant surface must result
in removal of that component.