Diamedica Baby CPAP Manual

Page 1 of 13
© Copyright Diamedica (UK) Ltd 2018
Diamedica Baby CPAP
INSTRUCTIONS FOR USE MANUAL
Diamedica (UK) Ltd
Grange Hill Industrial Estate
Bratton Fleming
Barnstaple, Devon
EX31 4UH, United Kingdom
Tel: +44 (0)1598 710066 Fax: +44 (0)1598 710055
Email: support@diamedica.co.uk www.diamedica.co.uk
Revision B 31-05-2018 DCN-0012
ENG
0088

Page 2 of 13
© Copyright Diamedica (UK) Ltd 2018
Read this page first
INTENDED USE
This device is suitable for use in hospital settings with limited resources or in any field or outreach
locations (where a suitable power source is available) and is suitable for neonate and paediatric
patients.
The Diamedica CPAP provides effective and efficient non-invasive airway pressure support to
neonate and paediatric patients in difficult environments.
FOREWORD
This manual is intended to provide guidance on the function, performance and user maintenance
of the Diamedica Baby CPAP. The information given in this manual is correct at the date of
publication.
A Separate IFU manual for the oxygen concentrator is also included and must be reviewed for
specific safety and maintenance requirements before use.
The policy of Diamedica (UK) Ltd is to continuously improve its products. Changes may be made to
this manual without notice being given.
Users of the Diamedica Baby CPAP must read, understand and follow the guidance given in this
manual before using the system.
THE NEED FOR PATIENT MONITORING
WARNING
The Diamedica Baby CPAP delivers mixtures of oxygen-enriched air to the patient and the device
should be monitored at all times.
It is essential that the patient’s oxygen saturation and other vital functions are also monitored.
The ultimate responsibility for patient safety remains with the operator.
Observations of the patient must take precedence over machine settings in judging the condition
of the patient.
The system is only intended for use by competent medical personnel

Page 3 of 13
© Copyright Diamedica (UK) Ltd 2018
Figure 1. The CPAP Concentrator
Oxygen concentrators are machines that extract nitrogen from atmospheric air, resulting in an
output of almost pure oxygen. CPAP is continuous positive airway pressure, which can assist
children with severe respiratory distress. The bubble-CPAP concentrator delivers both oxygen and
continuous positive airway pressure, the level of which depends on the distance the tubing is
under the water in the bottle.
Main gas outlet
Expiratory limb
Humidifier bottle
Bottle with dial-up
CPAP level
Air flow meter
Oxygen flow meter
Hour meter
Oxygen / Air mixing
chart
Start button
Inspiratory limb
Only persons who have read and understood this entire manual and
therefore deemed competent, are authorized to operate this equipment
Surge protector
Water Trap
Oxygen warning light

Page 4 of 13
© Copyright Diamedica (UK) Ltd 2018
Setting Up the Bubble-CPAP Concentrator
Follow the steps below to use the bubble-CPAP concentrator:
1. Position the concentrator so that it is at least 30 cm away from walls or curtains, so that the
inlet opening at the back is not obstructed.
2. Plug the power cord into the mains electricity supply, and turn on the concentrator.
3. Switch on the concentrator (switch on the console). A yellow light should turn on and remain
lit for a few minutes (usually within 10 minutes) until the concentration of the gas supplied
reaches and exceeds 85± 3% O₂. The yellow light should then turn off after this time, showing
that the concentrator is running correctly.
4. Fill the bottle to the level indicated with boiled water that has been allowed to cool, and screw
the lid back on.
5. Connect the inspiratory limb of the circuit to the main gas outlet.
6. Connect the expiratory limb of the circuit to the bottle.
7. Dial up the level of CPAP required: start at 7 cmH2O (see figure below)
Bottle with dial-up
CPAP level
Expiratory limb

Page 5 of 13
© Copyright Diamedica (UK) Ltd 2018
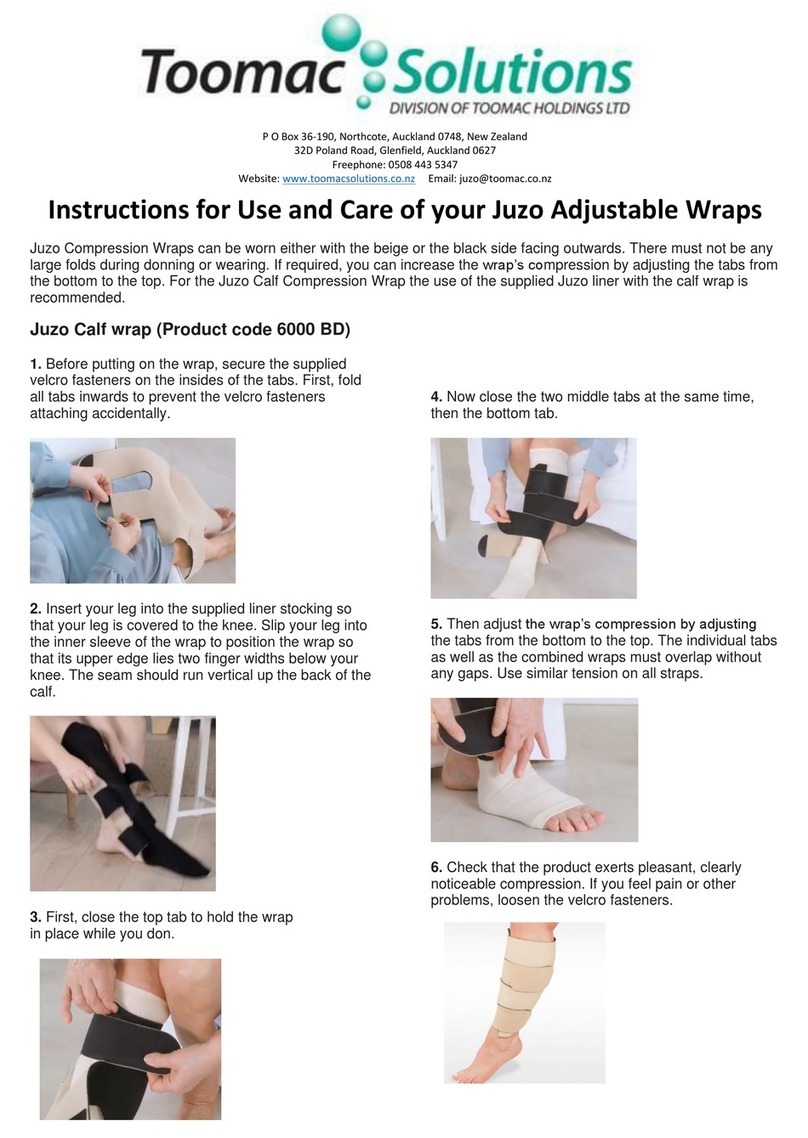
8. Connect the nasal prongs to the child as below:
a)
Place the bonnet on
patients head, centering
the “securement line
indicator”
b) With the bonnet
centered at nape of neck,
place remaining bonnet
on infant
f)
Attach chin strap to
the infant and secure
to Velcro
c)
Close the top of bonnet by
twisting bonnet until
tightly secure to head
crown.
d) Secure with ribbon
provided
g)
Place the nasal
prong into the
infants nostril
e) Cut self-adhesive Velcro in
half and secure to the
bonnet
h) Secure tubing by
placing elastic strap
over tubing and secure
to Velcro. Elastic strap
is correctly positioned
when strap is in line
within the securement
line indicator
9. Dial the flows of air and oxygen required to see a constant stream of bubbles in the water.
Start with 5 L/min of oxygen and 5 L/min of air. Check and record the flows dialled and the
oxygen concentration this provides. A total flow of 10 L/min is sufficient in most cases to
deliver CPAP, which you can see by continuous bubbling in the bottle.
10. Check the child for signs of respiratory distress, check the SpO2, and check if there are bubbles
in the bottle.
a. If the SpO2 is below 90% or the child has severe respiratory distress, first increase
the CPAP level to 8 or 10cmH20 and then, if no response the oxygen flow meter to
as much as 8 L/min.
b. If there are not continuous bubbles, check the nasal prongs are attached properly,
and reposition them so they fit snugly inside the nostrils.
c. If there are still not continuous bubbles, check for leaks along the circuit, and adjust
the oxygen or air flows according to the chart below.

Page 6 of 13
© Copyright Diamedica (UK) Ltd 2018
SpO2 >90% and
mild or no
respiratory distress
SpO2 >90% but
moderate to severe
respiratory distress
SpO2 <90%
Bubbles No immediate
change needed,
may be able to
reduce CPAP level
to 5 cmH20
Increase CPAP level Increase CPAP level
Increase oxygen
flow
No bubbles Check nasal
interface
Wean CPAP level
and check if child
still needs CPAP
Check nasal interface
Increase air flow,
check for bubbles
Increase CPAP level
Check nasal
interface
Increase oxygen
flow, check for
bubbles
Increase CPAP level
Trialling patients off CPAP and when to stop CPAP
At least once each day, children in the ward who are clinically stable (have no emergency signs and
SpO2 >90%) should be disconnected from CPAP for 10–15 minutes, and carefully examined for
changes in clinical signs and SpO2, to assess whether supplemental oxygen and CPAP is still
required. Trials off CPAP are best done first thing in the morning, when there is likely to be
adequate staff to observe the child throughout the day. If trials off CPAP are started in the late
afternoon, low staff numbers overnight and the oxygen desaturation that sometimes occurs
during sleep mean that there is a risk of hypoxaemia developing unrecognized overnight.
Children who have an SpO2 <90% while still on CPAP or who are unstable or very unwell should
not be given trials on room air.
Before a trial off CPAP, the SpO2 should be checked to determine if the trial is safe
(i.e. SpO2 >90%). The child should then be disconnected from the oxygen source and observed
carefully to avoid any adverse complications of hypoxaemia. If severe hypoxaemia (SpO2 <80%),
apnoea or severe respiratory distress occurs, children should be immediately restarted on oxygen.
Some children will become hypoxaemic very rapidly when they are taken off oxygen, and this is a
marker of very severe disease and a high risk of death. Parents and nursing staff should be advised
to watch the child to see if he/she develops cyanosis or severe respiratory distress.

Page 7 of 13
© Copyright Diamedica (UK) Ltd 2018
If the SpO2 is 90% or more after a trial on room air, they should remain off oxygen and the SpO2
should be rechecked after one hour, as late desaturation can sometimes occur.
If the SpO2 on room air is <90% or there is severe respiratory distress they should go back on
CPAP.
Any child who appears to deteriorate clinically should have their SpO2 checked to determine
whether they need oxygen. Children with acute respiratory disease should not be discharged until
their SpO2 has been stable at 90% or more while breathing room air for at least 24 hours, until
danger signs have resolved, and until appropriate home treatment can be organized.
Cleaning of the Circuit Tubing and Bottle
This is essential to reduce the risk of cross-infection. This should be done after every patient has
used the CPAP, and weekly if the same child is on CPAP for over a week. A spare circuit is essential
to replace the one that is being cleaned without interruption to the child’s treatment.
The CPAP circuit (inspiratory and expiratory limb, bottle and lid and connections) must be
thoroughly cleaned as follows:
1. Wipe off any gross soiling. Clean first with detergent (soap) to remove gross contamination
(e.g. blood, sputum);
2. Rinse with water that has been boiled and allowed to cool to tepid. Let it dry
3. Disinfect before re-using.
• Staff cleaning the equipment must wear protective clothing to avoid splash exposure or
contact with dirty equipment: wear apron, gloves and glasses.
• Good ventilation of the area is needed where you are cleaning the equipment
What You Need:
• Soap for initial clean
• Disinfectant solution: (sodium hypochlorite 0.05% or household bleach, diluted to
0.05% hypochlorite. The household bleach bottle will indicate its strength, dilution is
essential)
• Sink or buckets to clean equipment
• Brush to clean both inside and outside of circuit. All brushes and cleaning implements
must be properly cleaned after use – soap water and drip dry
• Gown or waterproof apron, mask and water-proof gloves
• Drying rack

Page 8 of 13
© Copyright Diamedica (UK) Ltd 2018
How to Wash and Disinfect
1. Wash hands
2. Prepare detergent (soapy water) and disinfectant solution wearing personal protective
equipment (PPE): gown or impermeable apron as a minimum, eye protection and
surgical mask for bleach solution
3. Wash first in soapy water, to remove blood and respiratory secretions. In clean sink or
bucket brush the equipment under water to prevent splash and ensure all visible soiling
is removed, rinse with water that has been boiled but allowed to cool to tepid
4. Let dry
5. Wash next in diluted bleach or disinfectant. Bleach needs one hour of soaking. Soak all
items together, do not keep putting one in and taking one out. Once used bleach
should not be re-used or kept in storage, discard after use.
6. Rinse with water that has been boiled and cooled to tepid (rinse also inside, for
example, using a sterile syringe), let it drip dry over the sink, do not leave it coiled on
the sink.
7. Remove all protective gear (apron, gloves, mask) and wash hands thoroughly
8. Check that there is no pooled water in the circuit. Store the circuit and bottle in a clean
plastic bag (labeled and dated). Store in the dry and clean area (separate from a soiled
equipment area)
Routine Cleaning and Maintenance of the CPAP-Concentrator
Each week the oxygen concentrator will require approximately 30 minutes of attention.
Concentrators have a large particulate filter over the air inlet opening (usually at the back of
freestanding or portable models). This filter stops dust and other airborne particles from entering
the unit. The filter should be removed and cleaned in warm soapy water, completely dried with an
absorbent towel and replaced. Have a spare dry filter to replace with so there are minimal
interruptions to the concentrator function.
The exterior of the oxygen concentrator should be cleaned with a mild disinfecting cleaning agent
or a diluted solution of bleach (usually 5.25% sodium hypochlorite). A solution in the range of
1:100 to 1:10 of bleach to water can be used effectively. Allow the solution to remain on the
surface for 10 minutes and then rinse off and dry.
Accessories and spares
All accessories used with the Baby CPAP must:
Be oxygen compatible,
Be biocompatible,
Comply with the general requirements of the 93/42/EEC European Directive
A full list of available spares is available by contacting Diamedica – [email protected]

Page 9 of 13
© Copyright Diamedica (UK) Ltd 2018
Method for disposing of the device
If the product is returned to the manufacturer at the end of its life the company will ensure
disposal in line with the Waste Electrical and Electronic Equipment Directive (WEEE) 2012/19/EU
An additional water trap may be
added to remove condensed
water from the system

Page 10 of 13
© Copyright Diamedica (UK) Ltd 2018
Instructions For Use – Additional information
This Baby CPAP unit has been fitted with an AVS30 Voltage Stabilizer to automatically protect the
on-board circuitry from damage due to unstable voltage.
The AVS30 is an Automatic Voltage
Switcher rated at 30 Amps. The AVS30 will
switch off the equipment connected to it if
the mains power goes outside pre-set
acceptable limits, and will reconnect
automatically when
the mains power returns to normal.
Reconnection takes place after a
delay, to ensure stability of the mains.
OR
OR
Input good
GREEN LIGHT
Power OK
Input unstable
RED LIGHT
No Power
Input now good
AMBER LIGHT
No Power for 10
seconds
Input good for 10
seconds
GREEN LIGHT
Power OK

Page 11 of 13
© Copyright Diamedica (UK) Ltd 2018
DIAMEDICA (UK) LTD
Grange Hill Industrial Estate, Bratton Fleming
Barnstaple, Devon, EX31 4UH, UK
Tel : +44(0)1598 710066
Email : support@diamedica.co.uk
www.diamedica.co.uk
0088

Page 12 of 13
© Copyright Diamedica (UK) Ltd 2018
SYMBOLS GLOSSARY
Some or all the following symbols may be used within this manual or found on the product or
packaging labels. Please familiarize yourself with them:
Symbol Description Comment
Manufacturer Indicates the medical device manufacturer,
as defined in EU Directives 90/385/EEC,
93/42/EEC and 98/79/EC.
Authorized
representative
in the European
Community
Indicates the Authorized representative in
the European Community.
Date of
manufacture
Indicates the date when the medical device
was manufactured.
Use-by date Indicates the date after which the medical
device is not to be used.
Batch code This symbol shall be accompanied by the
manufacturer's batch code. The batch code
shall be adjacent to the symbol.
Catalogue
number
Indicates the manufacturer's catalogue
number so that the medical device can be
identified.
Serial number Indicates the manufacturer's serial number
so that a specific medical device can be
identified.
Fragile, handle
with care
Indicates a medical device that can be
broken or damaged if not handled carefully.
Keep dry Indicates a medical device that needs to be
protected from moisture.

Page 13 of 13
© Copyright Diamedica (UK) Ltd 2018
Do not re-use Indicates a medical device that is intended
for one use, or for use on a single patient
during a single procedure.
Consult
instructions for
use
Indicates the need for the user to consult
the instructions for use.
Caution Indicates the need for the user to consult
the instructions for use for important
cautionary information such as warnings
and precautions that cannot, for a variety of
reasons, be presented on the medical
device itself.
Non-sterile Indicates a medical device that has not
been subjected to a sterilization process.
Class II equipment
Type BF applied
part
Recycling symbol Products with this symbol should not be
disposed of in the bin
The battery
recycling symbol
Chemical symbol for battery type included
beneath
Does not contain or
Have the presence
of natural rubber
latex
Indicates that an
object is capable of
being recycled
Table of contents
Other Diamedica Medical Equipment manuals