Boston Scientific L110 Quick start guide
Other Boston Scientific Medical Equipment manuals
Boston Scientific
Boston Scientific ENDOTAK RELIANCE User manual
Boston Scientific
Boston Scientific EASYTRAK 2 IS-1 User manual
Boston Scientific
Boston Scientific DB-1110-C Manual

Boston Scientific
Boston Scientific Vercise DB-5572-1A Manual
Boston Scientific
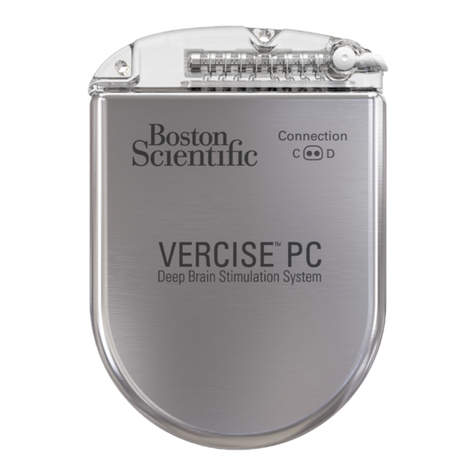
Boston Scientific Vercise PC Manual
Boston Scientific
Boston Scientific VERCISE DBS User manual
Boston Scientific
Boston Scientific Vercise DBS Leads Series Manual

Boston Scientific
Boston Scientific Swiss LithoClast Manual

Boston Scientific
Boston Scientific SC-4116 User manual

Boston Scientific
Boston Scientific SC-4108 User manual
Boston Scientific
Boston Scientific RELIANCE 4-FRONT DF4-LLHH User manual
Boston Scientific
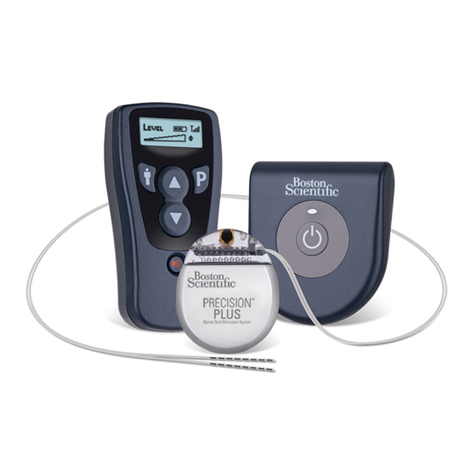
Boston Scientific Precision Spinal Cord Stimulator System Instructions for use
Boston Scientific
Boston Scientific Precision Spectra OMG SC-9315 User manual

Boston Scientific
Boston Scientific Rotablator Manual
Boston Scientific
Boston Scientific Precision SCS System Series Manual

Boston Scientific
Boston Scientific ENDOTAK RELIANCE Series User manual
Boston Scientific
Boston Scientific RELIANCE 4-FRONT Series User manual

Boston Scientific
Boston Scientific EndoChoice HedgeHog User manual

Boston Scientific
Boston Scientific DYNAGEN CRT-D User manual

Boston Scientific
Boston Scientific WaveWriter Alpha Owner's manual
Popular Medical Equipment manuals by other brands

Getinge
Getinge Arjohuntleigh Nimbus 3 Professional Instructions for use

Mettler Electronics
Mettler Electronics Sonicator 730 Maintenance manual

Pressalit Care
Pressalit Care R1100 Mounting instruction

Denas MS
Denas MS DENAS-T operating manual

bort medical
bort medical ActiveColor quick guide

AccuVein
AccuVein AV400 user manual

























