settings on the quality assurance record. These setting should be used for subsequent
testing.
5. Move the transducer slightly until the smallest anechoic group of targets is clearly
displayed. Freeze the display and obtain a hard copy.
6. Examine the group of targets displayed, to determine which target is the most clearly
displayed as compared to the adjacent targets. This target represents the focal zone.
Using the electronic calipers, obtain a depth measurement of this target. You will note,
the targets above and below this point become progressively fuzzier the further the
target is positioned from the focal zone.
7. Document the depth of the focal zone on the quality assurance record.
Results
The location of the focal zone should agree with the manufacturer's specifications and
should not change with time. The changeable focal zones should be verified for proper
operation of the multi-focal zone button. If changes occur corrective action should be
considered.
SENSITIVITY (MAXIMUM DEPTH OF PENETRATION)
Description and Reason For Testing
The ability of an imaging system to detect and display weak echoes from small objects
located at specified depths (penetration) is referred to as sensitivity. Clinically, weak
reflecting echoes are commonly produced from internal structures of organs. Definition
of these structures can be extremely important in the interpretation of the ultrasound
findings.
Sensitivity can be affected by the pulser/receiver section of the system, the degree of
focusing of the transducer, attenuation of the medium, depth and shape (geometry) of
the reflecting object, and electromagnetic interference from the local surroundings.
Test Procedure
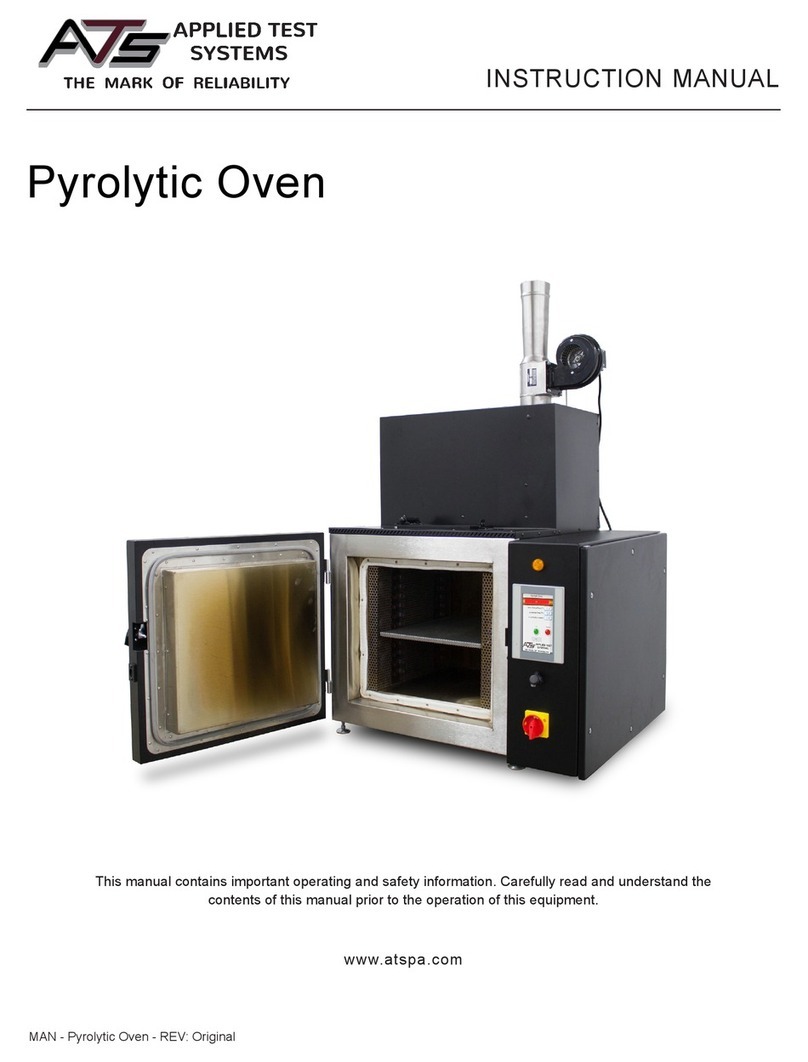
1. Place the phantom on a clean, flat surface with the internal scanning well positioned
for use.
2. Fill the scanning well slowly with water to avoid introducing air bubbles.
3. Insert the transducer into the scanning well.
4. Adjust the instrument settings (TGC, output, etc.) to establish baseline values for
"normal" liver scanning. If the bottom of the phantom is seen, adjust the gain settings
until the image fades and goes entirely black at the bottom of the display. Record these
settings on the quality assurance record. These setting should be used for subsequent
testing.