5
EN
Hemostatic agents applied at the wound site: Non-sutured hemostatic agents (for example, bone wax, absorbable
gelatin sponge, or spray wound sealant) may, if disrupted, increase the risk of bleeding, which, if uncontrolled, could be
potentially fatal. Protect against dislodging such agents. Consideration should be given to the negative pressure setting
and therapy mode used when initiating therapy.
Sharp edges: Bone fragments or sharp edges could puncture protective barriers, vessels, or organs causing injury. Any
injury could cause bleeding, which, if uncontrolled, could be potentially fatal. Beware of possible shifting in the relative
position of tissues, vessels or organs within the wound that might increase the possibility of contact with sharp edges.
Sharp edges or bone fragments must be eliminated from the wound area or covered to prevent them from puncturing
blood vessels or organs before the application of therapy. Where possible, completely smooth and cover any residual
edges to decrease the risk of serious or fatal injury, should shifting of structures occurs. Use caution when removing
dressing components from the wound so that wound tissue is not damaged by unprotected sharp edges.
Infected wounds: Infected wounds should be monitored closely and may require more frequent dressing changes than
non-infected wounds, dependent upon factors such as wound conditions and treatment goals. Refer to dressing appli-
cation instructions for details regarding dressing change frequency. As with any wound treatment, clinicians and
patients/caregivers should frequently monitor the patient’s wound, periwound tissue and exudate for signs of infection,
worsening infection, or other complications. Some signs of infection are fever, tenderness, redness, swelling, itching,
rash, increased warmth at the wound or periwound area, purulent discharge, or strong odor. Infection can be serious,
and can lead to complications such as pain, discomfort, fever, gangrene, toxic shock, septic shock and/or fatal injury.
Some signs or complications of systemic infection are nausea, vomiting, diarrhea, headache, dizziness, fainting, sore
throat with swelling of the mucus membranes, disorientation, high fever, refractory and/or orthostatic hypotension, or
erythroderma (a sunburn-like rash).
If there are any signs of the onset of systemic infection or advancing infection at the wound site, contact a phy-
sician immediately to determine if therapy should be discontinued.
Osteomyelitis: The therapy system should NOT be initiated on a wound with untreated osteomyelitis. Consideration
should be given to thorough debridement of all necrotic, nonviable tissue, including infected bone (if necessary), and
appropriate antibiotic therapy.
Protect tendons, ligaments and nerves: Tendons, ligaments and nerves should be protected to avoid direct contact
with foam dressings. These structures may be covered with natural tissue, meshed non-adherent material, or bioengi-
neered tissue to help minimize risk of desiccation or injury.
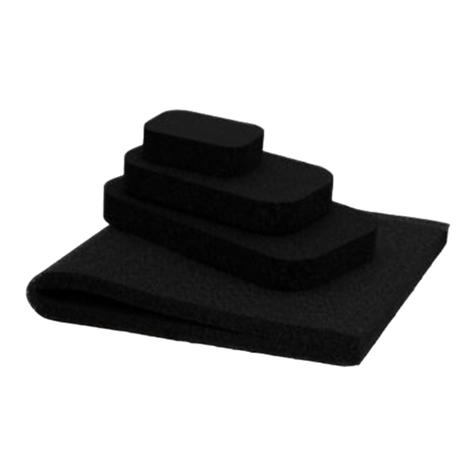
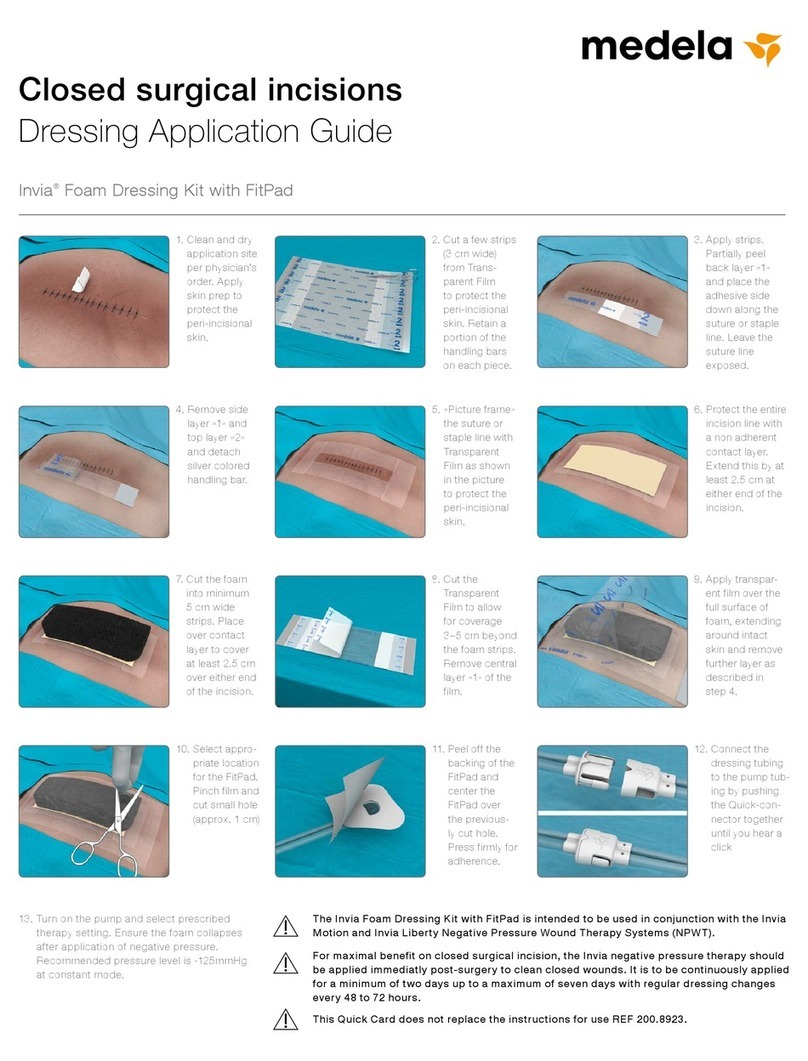
Foam placement: Always use dressings from sterile packages that have not been opened or damaged. Do not place
any foam dressing pieces into blind/unexplored tunnels. Do not force foam dressings into any area of the wound, as this
may damage tissue, alter the delivery of negative pressure, or hinder exudate and foam removal. Always count the total
number of pieces of foam used in the wound and document that number on the Transparent Film and in the patient’s
chart. Also document the dressing change date on the Transparent Film.
Foam removal: Foam dressings are not bioabsorbable. Always count the total number of pieces of foam removed
from the wound and ensure the same number of foam pieces was removed as placed. Foam left in the wound for
greater than the recommended time period may foster ingrowth of tissue into the foam, create difficulty in removing
foam from the wound, or lead to infection or other adverse events. Regardless of treatment modality, disruption of new
granulation tissue during any dressing change may result in bleeding at the wound site. Minor bleeding may be
observed and considered expected. However, patients with increased risk of bleeding, as described in the Warnings
section under Bleeding, have a potential for more serious bleeding from the wound site.
If significant bleeding develops, immediately discontinue the use of the therapy system, take measures to stop
the bleeding and do not remove the foam dressing until the treating physician or surgeon is consulted. Do not
resume the use of the therapy system until adequate hemostasis has been achieved and the patient is not at
risk of continued bleeding.
Acrylic adhesive: The Invia Transparent Film has an acrylic adhesive coating, which may present a risk of an adverse
reaction in patients who are allergic or hypersensitive to acrylic adhesives. If a patient has a known allergy or hypersen-
sitivity to such adhesives, do not use the therapy system. If any signs of allergic reaction or hypersensitivity develop,
such as redness, swelling, rash, urticaria, or significant pruritus, discontinue use and consult a physician immediately. If
bronchospasm or more serious signs of allergic reaction appear, seek immediate medical assistance.