Thoratec HeartMate II LVAS User manual

HeartMate II®LVAS
Clinical Operation
& Patient Management
Abbreviated and extracted from the HeartMate II®LVAS Operating Manual
© 2008 Thoratec Corporation
6035 Stoneridge Drive
Pleasanton, CA 94588
Tel. (925)847-8600, Fax. (925)847-8574
HeartLine™ (800)456-1477
www.thoratec.com
104185.A


Table of
Contents
INTRODUCTION................................1
Program Description.....................................1
Program Objective........................................1
Learning Objectives......................................1
SYSTEM OVERVIEW...................................2
Description....................................................2
Warnings & Precautions................................2
SYSTEM COMPONENTS.............................6
HeartMate II LVAD or “Blood Pump”..............6
How the Pump Works....................................6
·Pump Parameters..................................9
·Flow.......................................................9
·Power.....................................................9
·Pulsatility Index (PI)...............................9
·Operating Mode...................................10
PERIPHERAL COMPONENTS..................11
System Controller........................................11
Power Base Unit (PBU)...............................13
Batteries & Battery Clips..............................15
Emergency Power Pack (EPP)....................18
System Monitor...........................................18
Display Module............................................26
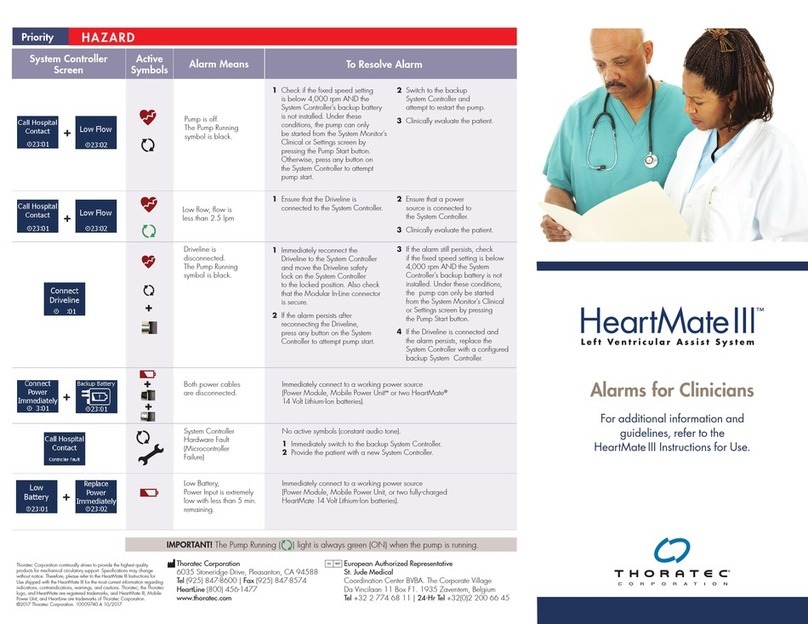
ALARM CONDITIONS................................27
ROUTINE OPERATING
PROCEDURES.........................................28
Changing from PBU to Battery-
Powered (Untethered) Operation................28
Changing from Batteries to PBU
(Tethered) Operation...................................30
Changing Batteries......................................32
Performing a System Controller
Self Test......................................................33
Changing the System Controller
Battery Module............................................34
Replacing System Controllers.....................35
HANDLING EMERGENCIES......................37
Defibrillation/Cardioversion.........................37
Cardiac Arrest.............................................38
PATIENT MANAGEMENT...........................39
Patient Assessment.....................................39
Potential Risks & Adverse Events...............39
Potential Late
Post-Implant Complications........................39
Caring for the Exit Site.................................40
Caring for the Percutaneous Lead...............40
Controlling Infection....................................41
Measuring Blood Pressure..........................41
Anticoagulation...........................................41
Activities of Daily Living...............................41
·Sleeping...............................................43
·Showering............................................44
THORATEC RESOURCES.........................45
Thoratec HeartLine™..................................45
Published Reference Materials...................45
POST TEST.................................................46
COMPETENCY ASSESSMENT
CHECKLIST................................................49
PROGRAM EVALUATION..........................50
NOTES........................................................51
CLINICAL OPERATION AND PATIENT MANAGEMENT
i

Introduction
Program Description
This inservice program reviews the theory of operation, function, components,
diagnostic monitoring, and related nursing management for the HeartMate II® Left
Ventricular Assist System (LVAS).
Program Objective
The primary objective of this inservice program is to supplement on-site education-
al programs. It is designed to help prepare clinicians for assuming care of patients
implanted with the HeartMate II LVAS.
Learning Objectives
After completing this program, participants should be able to:
1Identify the components of the HeartMate II LVAS, their functions, and the the-
ory of device operation.
2List two potential complications associated with a HeartMate II LVAS.
3Identify the purpose and function of each button and symbol on the HeartMate
II LVAS System Controller.
4Describe the procedure for changing a HeartMate II System Controller.
5Describe appropriate interventions in the event of an emergency.
CLINICAL OPERATION AND PATIENT MANAGEMENT
1

System Overview
Description
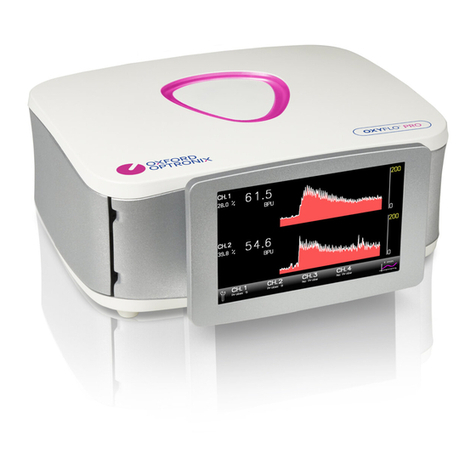
The HeartMate II is a left ventricular
assist system (LVAS) consisting of a blood
pump, external System Controller, and
external power supply components
(Figure 1). The HeartMate II is implanted
just below the heart. The flexible inflow
conduit is attached to the apex of the left
ventricle and the outflow graft is attached
to the ascending aorta. The HeartMate II
pumps blood from the weakened left ven-
tricle to the aorta. Both the inflow conduit
and outflow elbow feature textured
blood-contacting surfaces clinically
proven on the HeartMate XVE to be
thrombo-resistant.
Warnings and Precautions
General Warnings
· A thorough understanding of the technical principles, clinical applications, and
risks associated with left ventricular support is necessary before using this
product.
· Keep the Power Base Unit (PBU) away from water. If the PBU has contact with
water, shower spray, or wet surfaces, the pump may stop, or the patient may
receive a serious electrical shock.
· Do NOT use the PBU in the presence of flammable anesthetic agents or an
explosion could occur.
· Connect the PBU and any peripheral devices only to properly tested, grounded
and dedicated AC outlets. Do NOT use an adapter for ungrounded wall outlets
or multiple portable socket outlets (power strips), or the risk of electrocution
increases.
· Do NOT connect the PBU to an outlet controlled by a wall switch or the PBU
may be left inoperable.
· Do NOT use this device in pregnant women or any woman likely to become
pregnant during her period of LVAS support.A growing fetus will dislodge the
pump, which may result in device failure or fatal hemorrhage. In addition, anti-
coagulation regimens are contraindicated during pregnancy.
· Do NOT subject patients implanted with the HeartMate II LVAS to Magnetic
CLINICAL OPERATION AND PATIENT MANAGEMENT
2
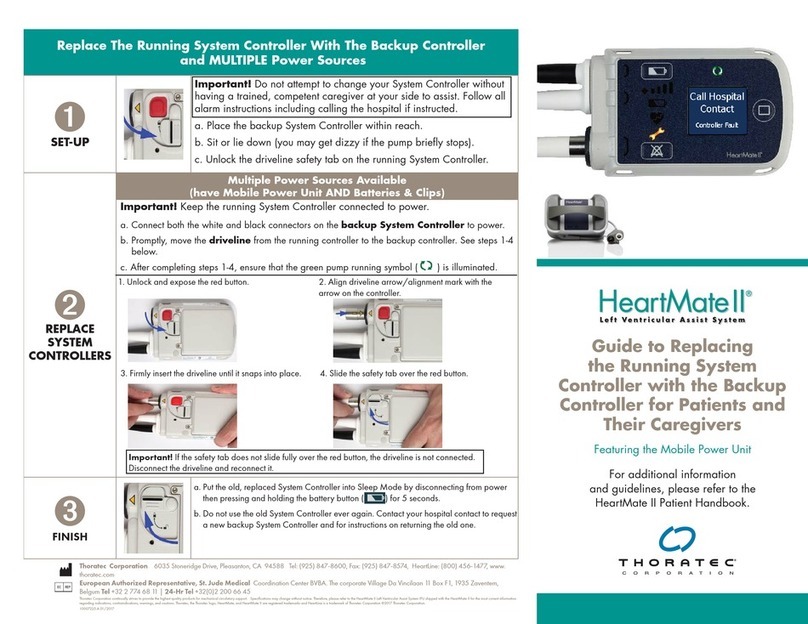
Figure 1 Implanted and worn components of the
HeartMate II LVAS (shown using battery power for unteth-
ered operation).

Resonance Imaging (MRI), as the pump contains ferro-magnetic components,
and MRI could cause device failure or patient injury.
· Do NOT apply high power electrical treatment (e.g., application of diathermy)
directly to the patient.
· Disconnecting the HeartMate II LVAS from the System Controller is advised
during open heart defibrillation due to the proximity of the paddles to the
device. However, the LVAS should NOT be disconnected during external defibril-
lation.
· The implanted components of the LVAS should NOT be exposed to therapeutic
levels of ultrasound energy (e.g., ultrasound heating and/or extracorporeal
shockwave lithotripsy) used to alter or albate tissues, as the device may inadver-
tently concentrate the ultrasound field and cause harm to the patient. This does
NOT apply to diagnostic techniques, such a echocardiography.
· Therapeutic ionizing radiation may damage the device, which may not be
immediately detectable.
· Avoid strong static discharges (e.g., from touching television or computer moni-
tor screens, vacuuming carpets, etc.) as this can damage the electrical parts of
the system and cause the LVAD to stop.
· To prevent device damage and personal injury, refer servicing to authorized
service personnel trained by Thoratec corporation.
Warnings Specific to Patient or System Management
· System components must never be immersed in water or liquid. Showers and
washing are permitted when the clinician approves wound site readiness.
During showers, the HeartMate Shower Kit must be used.
· In the event that the LVAD stops operating, attempt to restore pump function
immediately. In the event that the LVAD stops operating and blood is stagnant
in the pump for more than a few minutes (depending on the coagulation status
of the patient), there is a risk of stroke or thromboembolism should the device
be restarted. There is also the potential for retrograde flow within the LVAD.
· Disconnecting both System Controller power leads at the same time will result
in loss of pump function. One System Controller power lead must be connected
to a power source (i.e., batteries, PBU, or EPP) at all times to maintain support.
The following will cause the LVAD to stop and blood pumping to cease:
- Disconnecting both power leads from the PBU when operating on PBU
power.
- Removing both batteries from their respective battery clips when operating
on battery power.
- Completely depleting all battery charge when operating on battery power.
· Disconnecting the percutaneous lead from the System Controller will result in
loss of pump function. The System Controller must be reconnected as quickly
as possible to resume pump function:
CLINICAL OPERATION AND PATIENT MANAGEMENT
3

CLINICAL OPERATION AND PATIENT MANAGEMENT
4
-For pump speeds <8,000 (typical at time of device implantation), recon-
nect the System Controller and then firmly press the Silence Alarm or Test
Select button as quickly as possible to resume pump function.
-For pump speeds >8,000 (typical post implant), reconnect the System
Controller as quickly as possible to resume pump function. The pump
should automatically resume pumping once power is restored.
General Precautions
·RefertotheHeartMate II LVAS Instructions for Use and the HeartMate II LVAS
Operating Manual for detailed instructions and information on device implant
and system setup, function, and maintenance. These manuals are not intended
to replace comprehensive laboratory or educational programs, or to supercede
appropriate medical judgment, however.
· Patients with mitral or aortic mechanical valves may be at added risk of accu-
mulating thrombus on the valves when supported with left ventricular assist
devices.
· Only use Thoratec Corporation's PBU to charge batteries. Other battery chargers
may damage HeartMate batteries.
· Do NOT use batteries below 15oF (-10oC) or above 105o F (40oC) or they may fail
suddenly. If batteries are below room temperature (68-72oF, 20-23oC) during use,
their capacity will be reduced.At the low end of the temperature range (15o,-
10oC), run time will be reduced by 50%.
· Use of expired or defective batteries may result in reduced operating time or
abrupt loss of pump function.
· Dispose of expired, used, or damaged batteries according to local, state or feder-
al regulations. Do not incinerate.
· The use of other electronic devices (medical or non-medical) that do not com-
ply with the equivalent safety requirements of the PBU may lead to reduced
patient safety. When considering whether or not to use an electronic device on
or near the patient:
· Confirm that the safety certification of the accessory has been performed in
accordance to the appropriate IEC 60601-1 and/or IEC 60601-1-1 harmo-
nized national standard.
· Use only those devices necessary for patient safety and well-being.
· Do not store or use the Emergency Power Pack (EPP) below 32oF (0oC) or above
122oF (50oC) or it may fail suddenly. If the EPP is below room temperature (68-
72oF, 20-23oC) during use, it will run the pump for less than 10 hours.At the low
end of the temperature range (32o F, 0oC), run time will be reduced by 50%.
· To prevent deterioration or damage to the EPP:
· Do not leave or store the EPP in hot or cold areas (car trunk, etc.) or battery
life will be shortened.
· Do not use the EPP beyond the expiration date.
· Dispose of an expired, used, or damaged EPP according to local, state or fed-

eral guidelines. Do not incinerate.
· Avoid unnecessary pulling or moving of the external portion of the percuta-
neous lead, especially as the exit site is healing. Pulling on or moving the lead
could prolong the healing process or disrupt an already healed exit site.
Disruption of the percutaneous lead exit site increases the patient's risk of
acquiring a serious infection.
· Immobilize the external portion of the percutaneous lead at the exit site using
the HeartMate Stabilization belt. Immobilizing the percutaneous lead promotes
tissue ingrowth and exit site healing, which reduces the risk of exit site infec-
tion. The Stabilization Belt should be worn AT ALL TIMES.
· Connectors should be kept clean and dry. Do NOT expose connectors to water/
liquid when making or breaking connections.
· Avoid discharging static electricity to the System Controller or LVAD percuta-
neous lead.
· Never use tools to tighten connections. Hand tighten only. Using tools may dam-
age the connectors and cause the pump to stop.
Precautions Specific to Patient or System Management
· Diligent care throughout the course of LVAS support must be exercised to pre-
vent infection and sepsis. Systemic infections and localized infection of the per-
cutaneous lead exit site may occur with use of this device. Infection may con-
tribute to patient morbidity and death.
· The use of automated blood pressure monitoring devices may not yield accurate
blood pressure data. Manual ausculation to assess blood pressure is recom-
mended. In circumstances where the flow is not sufficient for ausculation,
Doppler or invasive blood pressure monitoring may be required.
· Right heart failure can occur following implantation of the device. Right ventric-
ular dysfunction, especially when combined with elevated pulmonary vascular
resistance, may limit LVAS effectiveness due to reduced preload to the LVAD.
· An ECG may be indicated to rule out fibrillation if a patient complains of feeling
"different".
· Reports of change in sounds and/or motion of the system by the patient should
prompt evaluation for cause, including the possibility of device malfunction.
· Physiological factors that affect preload to the pump, such as hypovolemia or
postural hypotension, will result in reduced pump flows as long as the condition
persists. Pump flows will not be restored to normal unless such conditions are
treated.
· When connecting leads, do NOT force together connectors without initial proper
alignment. Forcing together misaligned connectors may damage them.
· At least one set of fully-charged spare batteries and a backup System Controller
that has been programmed with the patient’s settings must remain with the
patient at all times for use in an emergency.
CLINICAL OPERATION AND PATIENT MANAGEMENT
5

System Components
HeartMate II system components include the implantable Left Ventricular Assist
Device (LVAD) or“blood pump” with its percutaneous lead, as well as the following
external peripheral components:
·SystemController
· Power Base Unit (PBU) and PBU cable
· Batteries and battery clips
· Emergency Power Pack (EPP)
· System Monitor
·DisplayModule
Note: The following is only an overview of major system components. Refer to the
HeartMate II LVAS Operating Manual for complete information.
HeartMate II LVAD or “Blood Pump”
The HeartMate II left ventricular assist
device (LVAD) or“blood pump” is a
continuous flow rotary LVAD (Figure
2). The LVAD has only one moving
part, a small spinning rotor that
receives power from the System
Controller.Vanes on the spinning rotor
move blood through the pump, which
is capable of providing flow from 3 to
10 liters per minute (lpm). The follow-
ing pump components that come in
contact with the blood have a smooth,
polished titanium surface: pump
rotor, stators, and pump chamber. The
pump’s inlet cannula, inlet elbow, and
outlet elbow have textured surfaces.
The HeartMate II’s patented ball-and-cup bearings are designed for long term relia-
bility and minimal blood damage. There are no valves in the HeartMate II.
The implanted pump lies parallel to the diaphragm in a sub-diaphragmatic posi-
tion. It may be implanted preperitoneally or intra-abdominally.
How the Pump Works
Blood flow through the HeartMate II LVAD follows the native cardiac cycle and will
vary during diastole and systole. Therefore, the HeartMate II LVAD is essentially
synchronized with the mechanical activity of the native heart and follows the Frank
CLINICAL OPERATION AND PATIENT MANAGEMENT
6
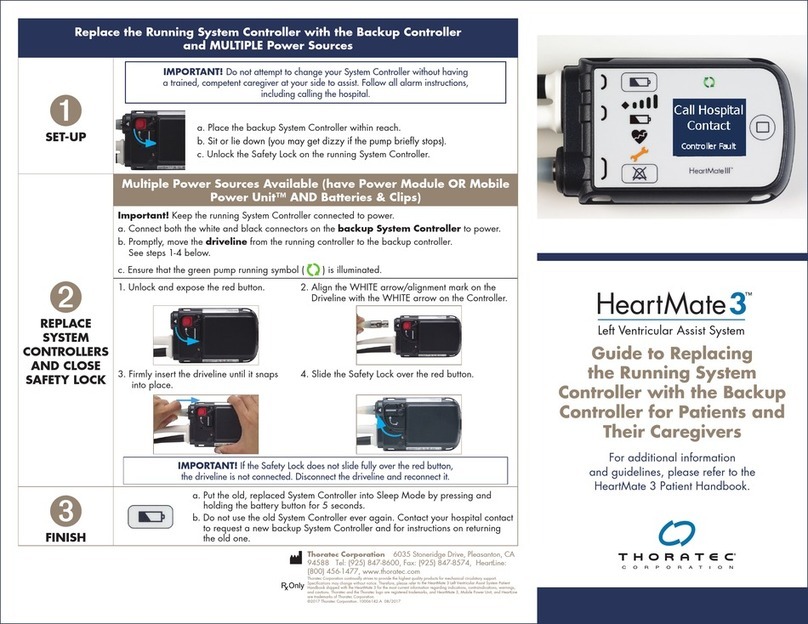
Figure 2 Implanted & worn components of the
HeartMate II LVAS
HeartMate II System
Controller
HeartMate II
LVAD

Starling Curve.
The amount of flow generated by the pump is determined by the pump speed and
by the pressure gradient that exists across the pump.“Pressure gradient” is defined
as the difference between the pressure at the pump outlet and pump inlet.
For a specified pump speed, flow varies inversely with pressure across the pump.
Therefore, increasing pump pressure differential (gradient) decreases flow, and
decreasing pump pressure differential increases flow. Hence, the dynamic parameter
that determines pump differential pressure is left ventricular pressure, which is
dependent upon the contractile state of the ventricle.
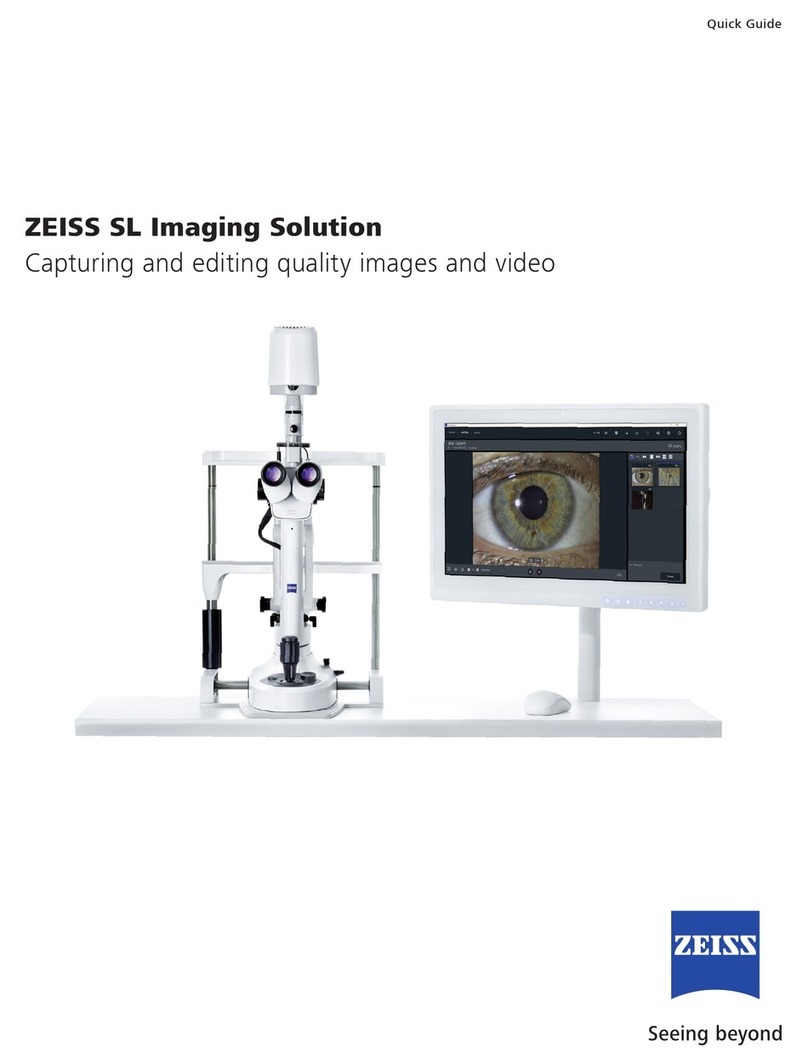
The simulated monitor tracings (Figure 3) show the ventricular and aortic pres-
sures of a patient:
· The blue waveform represents the pressure at the pump inlet, which is the left
ventricular or LV pressure.
· The red waveform represents the pressure at the pump outlet, which is the aor-
tic pressure.
· The difference between these two pressures, indicated by the vertical yellow bar,
is the pressure difference across the pump. This difference varies over the car-
diac cycle, with the largest pressure difference occurring in ventricular diastole
and the smallest pressure difference occurring during ventricular systole.
CLINICAL OPERATION AND PATIENT MANAGEMENT
7
Figure 3 Tracings showing ventricular and aortic pressures

For a given pump speed, in this case 8,000 rpm, the differential pressure defines
what the flow through the pump will be at any given moment.
In other words, during cardiac systole the blue waveform (LV pressure) rises and is
essentially identical to the red waveform (aortic pressure), which results in a
decrease in the differential pressure (gradient) and increased pump flow. As the
pump inlet and outlet pressures become more equalized, it becomes easier for the
pump to propel blood forward. The reverse is true during diastole at the same pump
speed, where the blue waveform (inlet pressure) and red waveform (outlet pressure)
separate, shown by the yellow bar. When this occurs, the differential pressure rises
and the pump must overcome this increased pressure difference between LV and
aortic pressure in order to propel blood forward; therefore flow decreases.
As pump speed increases, the aortic tracing and flow through the pump becomes
less pulsatile as demonstrated in the tracings below (Figure 4a and 4b).
CLINICAL OPERATION AND PATIENT MANAGEMENT
8
Figure 4a Aortic tracing and flow through pump at pump speed of 9,000 rpm and pulsatility
index (PI) of 2.4
Figure 4b Decreased pulsatility (PI 0.4) when pump speed is increased to 10,000 rpm

Pump Parameters
The system-provided parameters of speed, power, flow, and pulsatility index (PI), in
conjunction with echocardiography, serve as the primary indicators of device func-
tion. Once baseline values representing a satisfactory level of patient support are
established, the degree of change in a parameter usually has more clinical signifi-
cance than its absolute value. No single parameter is a surrogate for monitoring the
clinical status of the patient, and changes in all parameters should be considered
when assessing a situation.
Flow
Flow is directly related to speed and power.As the fixed speed is increased, flow will
increase. Pump flow is not directly measured but is an estimated value based on
pump power.Any increase in power will result in an increase in estimated flow.Any
condition that causes an increase in pump power not related to increase flow, such
as thrombus on the bearings or obstruction of the rotor, will display an erroneously
high flow.
Power
The amount of power used by the pump is determined by pump speed and blood
flow through the pump. Under normal conditions, the power increases with either
pump speed or flow. Gradual power increases (over hours or days) may signal a
deposition of thrombus inside the pump. Depending on the speed, power values
greater than 10 to 20 watts may also indicate the presence of a thrombus.Abrupt
changes in power, more than 2 watts, not accompanied by a change in pump speed
should also be evaluated.
Pulsatility Index (PI)
The pulse index, or “PI,” is a measure of the magnitude of the flow pulse through
the pump during the cardiac cycle. It is measured and averaged over a 15-second
interval and displayed on the monitor.
PI = Max Flow - Min Flow X 10
Average Flow
Factors that affect PI are LV preload or contractility and pump speed. When preload
increases in the native left ventricle, the Starling Curve is affected (i.e., increased
contractility) and pulsatility increases. When preload decreases, PI decreases. Pump
speed is inversely related to PI. As pump speed is increased, the LV is unloaded with
a decrease in preload, resulting in a lower PI value. Conversely, decreasing pump
speed increases LV preload, resulting in a higher PI value.
Note: Even a severely depressed heart has some residual rhythmic contraction; and,
any contraction will create a pressure pulse. Thus, under most circumstances, sys-
temic flow is pulsatile. It takes a completely flaccid heart or one in fibrillation to
have no ventricular contribution to the pulse at all.
CLINICAL OPERATION AND PATIENT MANAGEMENT
9

Operating Mode
The System Controller has a single primary operating mode, called fixed speed
mode, which maintains operation at a constant pump speed between 6,000 and
15,000 rpm. The typical range is 8,000 to 10,000 rpms. Pump speed is adjustable in
increments of 200 rpm.Adjustments can only be made through the System Monitor.
CLINICAL OPERATION AND PATIENT MANAGEMENT
10

Peripheral Components
System Controller
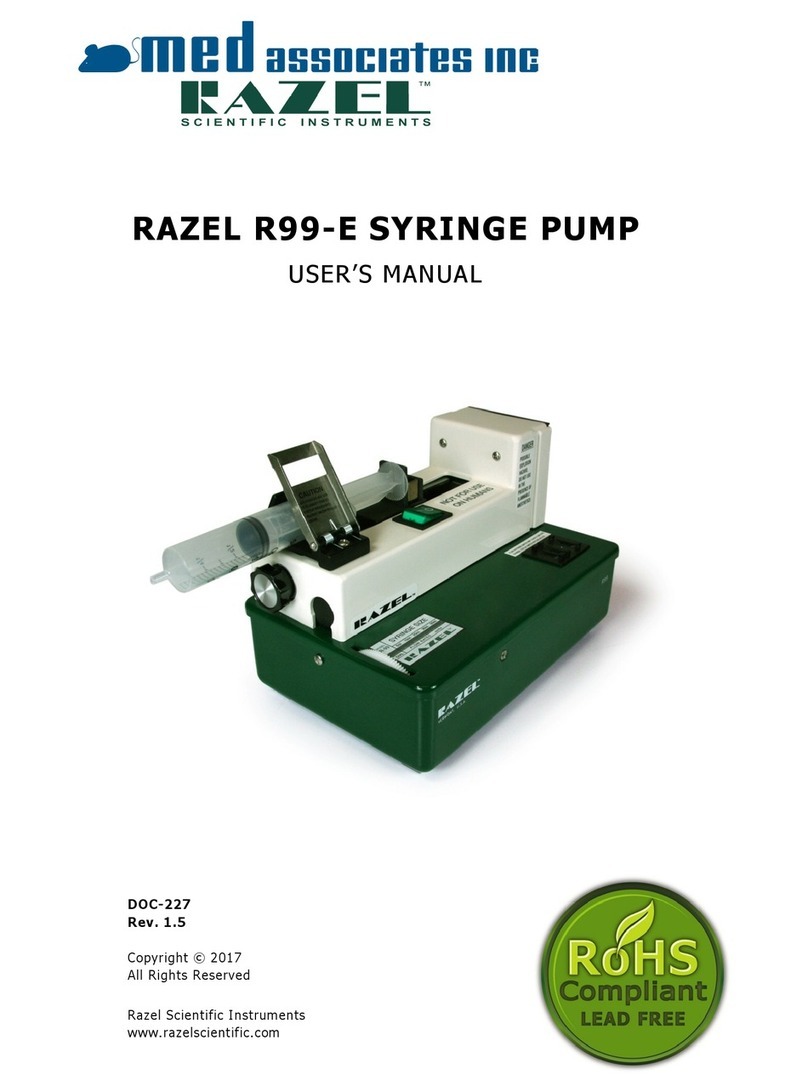
The HeartMate II System Controller (Figure 5) controls LVAD operation and serves
as the primary user interface of the HeartMate II LVAS.
The System Controller performs the following functions:
- Controls motor power and speed.
- Provides redundant system operation.
- Monitors, interprets, and responds to system performance.
- Performs diagnostic monitoring.
- Provides hazard and advisory alarms.
- Records and stores events in memory.
- Transfers system performance data to the System Monitor or Display Module.
The System Controller contains two computer boards. One provides primary system
operation and the other provides complete backup system operation in the event
the primary system malfunctions.
The System Controller has two power leads (one with a black connector and one
with a white connector) that connect the System Controller to its power source.
While both leads provide equal power, the white lead contains a data link cable that
transmits information from the System Controller to the System Monitor or Display
Module during tethered operation. A battery inserted into the side of the Controller,
called the System Controller alarm battery module, provides limited power to the
System Controller’s audible alarms during situations when external power has been
disrupted. The System Controller alarm battery module does not provide backup
power to the System Controller or pump
CLINICAL OPERATION AND PATIENT MANAGEMENT
11
Figure 5 HeartMate II LVAS System Controller with Leads (note black and white connectors)
WARNING ! The System Controller alarm battery module only provides power to the
Controller’s audible alarm tones. It does NOT provide power to the Controller or pump.

The System Controller keypad (Figure 6) has a Silence Alarm button and a Test
Select button, both of which can be used to interact with the system. Either button
can be pressed and held for two seconds to restart the pump if the System
Controller does not automatically do so (for instance, if the percutaneous lead
and/or power leads are disconnected from the the System Controller and the fixed
speed setting is below 8,000 rpm). These two buttons can also be used to force the
System Controller into backup system operation by pressing both simultaneously
when the pump is off or not connected to the Controller. The Silence Alarm and Test
Select buttons are described in more detail below.
Silence Alarm Button
The Silence Alarm button has two main purposes: to display the battery fuel gauge
and to silence audio alarms.An audio alarm is silenced for two minutes if a hazard
condition or Power Cable Disconnected advisory is active; and, for four hours if
general advisories are active. If the alarm condition resolves within this period, the
alarm will not recur.While the audio alarm is silenced, the respective alarm sym-
bol(s) flash(es) as a reminder that the alarm condition remains active.
When the patient is tethered to the PBU, the PBU repeats (duplicates) a System
Controller audible alarm. This second alarm can be silenced for five minutes using
the Alarm Reset button on the PBU front panel; or, to silence both the Controller
and the PBU, press the Silence Alarm button on the System Controller or System
Monitor screen.
Repeated attempts to prolong the silence period by pushing the Silence Alarm but-
ton will not add time to the silence period.Any new hazard or advisory alarm condi-
tions arising during the four hour silence period will initiate a new visual and audio
alarm. Only a new hazard alarm condition arising during a two minute silence peri-
od will initiate a new audio alarm.Audible advisory alarms will not occur until the
hazard or power cable disconnected alarm has been resolved.
Test Select Button
The Test Select button is used to initiate a system controller self-test. The self-test
CLINICAL OPERATION AND PATIENT MANAGEMENT
12
Test Select
Button
Battery Symbol
(yellow & red)
Battery Fuel Gauge
Power Symbol
(green)
Controller
Battery Module
(yellow)
Red Heart
Symbol
Silence
Alarm
Button
Figure 6 System Controller Keypad

should be performed daily. Refer to Performing a System Controller Self Test located
on page 33 for instructions .
System Controller Event Recorder
The System Controller event recorder automatically captures data when an alarm
event occurs.
The System Controller data logger can be set up via the System Monitor Save Data
Screen to record data at designated intervals of 30 minutes, or hourly from one to 24
hours. The Controller can record up to 120 events, which includes events that occur
during alarm conditions and at pre-set intervals.
Power Base Unit (PBU)
The Power Base Unit (PBU) (Figure 7)
provides AC power to the LVAD when the
patient is connected to it via the 20-foot PBU
cable; this is referred to as tethered operation.
The PBU can charge up to six batteries in
eight hours or less, depending on the charge
status of the batteries. Battery charging can
occur simultaneously with tethered operation.
The PBU has six battery charging stations;
each station has three charge indicator lights that indicate a battery’s charge status.
To charge or test a battery, slide the battery into the slot with its metal terminal fac-
ing up.When the battery is in place, the yellow light will illuminate while the PBU
performs a 10-second load test. After testing, one of three lights will illuminate to
indicate the status of that battery (see Table 1).
CLINICAL OPERATION AND PATIENT MANAGEMENT
13
Battery is fully-charged and ready for use.
Note: Battery will not be damaged if left in the PBU after
becoming fully-charged.
Ten-second load test is being performed. Note: If light
remains yellow after test, battery is being charged and thus
is not yet ready for use. The light will turn green once the
battery becomes fully-charged (see above).
Battery may be improperly positioned in slot. Reinsert into
same slot to attempt second test.
If the battery fails the second test, remove the battery and
clean the battery terminal with a lint-free cloth that has been
moistened with rubbing alcohol. Allow the alcohol to dry, then
reinsert the battery into a different slot.
If it fails again, battery is defective and should be replaced.
Do NOT use defective batteries.
Note: If battery shows red light in one slot but yellow or green
in another slot, consult Thoratec’s Field Service Department.
Green
Yellow
Red
Table 1 Battery Load Test Status
Battery Charge Indicators
Figure 7 Power Base Unit (PBU) Front Panel

The patient should be connected to the PBU when sleeping or anticipating sleep.
The PBU also echoes (duplicates) alarms that are generated by the System
Controller. Note: The PBU, like any piece of electrically-powered life-sustaining
equipment, should remain continually plugged into a properly-grounded (3-prong)
AC mains electrical outlet, except during transport or service.
Power Base Unit (PBU) Alarms
AC FAIL Alarm
In the event of AC mains power failure, the PBU’s AC Fail alarm will activate.
The AC Fail alarm is indicated by the illumination of a RED LIGHT on the
PBU’s front panel (Figure 8) accompanied by a CONTINUOUS AUDIO TONE.
In response to this condition, the PBU will automatically revert to its internal
backup battery to power the LVAD for approximately 30 minutes and the
patient should promptly switch from tethered (PBU-powered) operation to bat-
tery-powered or EPP operation until AC power is restored.
Note: Batteries in the PBU battery charging slots will not lose their charge dur-
ing AC mains power failure; however, neither will they continue to charge dur-
ing this time.
Pressing the Alarm Reset switch below the RED LIGHT on the PBU will silence
the AC Fail alarm until the low battery alarm is activated.
Lo Batt Alarm
When the internal backup battery in the PBU has 10 minutes of battery power
remaining, the PBU’s low battery alarm (ie,“Lo Batt” Alarm) will activate. The
Lo Batt Alarm is represented by a RED LIGHT and a CONTINUOUS AUDIO
TONE.
When the System Controller power leads are connected to the PBU cable and
the LVAD is operating in tethered operation this alarm cannot be silenced. It
will continue until AC power has been restored to the PBU, the internal battery
is completely depleted, or the patient is switched to batteries. In response to
this condition, the patient should be changed immediately from tethered oper-
ation (PBU-powered) to battery-powered operation.
Note: PBUs are shipped to customers with the internal battery disconnected.
CLINICAL OPERATION AND PATIENT MANAGEMENT
14
Figure 8 Power Base Unit (PBU) Front Panel

Upon receipt of the PBU, the hospital’s biomedical technician or other author-
ized and trained personnel must open the PBU and connect its internal battery
prior to set up and use. To confirm that the PBU’s internal battery has been
installed and properly charged, turn off the PBU power switch or unplug the
PBU power cord from the socket and verify that the the AC fail alarm sounds
for longer than 10 seconds and that the AC fail LED light is illuminated.
Batteries & Battery Clips
Batteries
A pair of wearable, rechargeable HeartMate batteries (Figure 9) will power the
HeartMate II LVAD for approximately 3-5 hours, depending on the charge status of
the batteries and the hemodynamic condition of the patient. Round Velcro® indica-
tors are supplied with each battery to designate a battery’s charge status. For exam-
ple, when a battery is fully charged, place the indicator on the battery white-side-up;
when it’s depleted, turn over the indicator and place it black-side-up (Figure 9).
To minimize deterioration or damage to batteries:
· Do NOT drop or subject batteries to strong physical shock.
· Do NOT leave or store batteries in hot areas or battery life will be shortened.
· Do NOT use batteries in temperatures below 15oF (-10oC) or above 105oF (40oC)
or they may suddenly fail.
· Do NOT connect the negative and positive battery terminals.
· Recharge used batteries within 12 hours or battery life may be shortened.
CLINICAL OPERATION AND PATIENT MANAGEMENT
15
WARNING ! Use of expired or defective batteries may result in reduced operating time or
abrupt loss of LVAD function.
Figure 9 HeartMate Batteries with Charge Status Indicators
WARNING ! There are no backups for this system. In the event that the LVAD stops
operating, all attempts should be made to restore pump function immediately. Loss of
power will cause the LVAD to stop and blood pumping to cease. Power must be
restored immediately. In the event that the LVAD stops operating, retrograde flow may
occur; and, if non-circulating blood is in the pump for more than a few minutes (depend-
ing on the coagulation status of the patient), there is a risk of stroke or thromboem-
bolism should the device be restarted.

Battery Clips
Before connecting the batteries to the System Controller, each battery must be
inserted into a HeartMate battery clip (Figure 10). Note:Batteryclipshaveanelec-
trical connection for attaching the Controller power leads. One battery is inserted
into each clip (match black arrow on battery with black arrow on clip). The battery
clicks into place when properly inserted. Press the spring-loaded release button to
release a battery from its clip.
NEVER disconnect both leads from batteries at the same time, or the pump will
stop. This could result in serious patient injury or death. After reconnecting power,
the pump will automatically restart if the fixed speed setting is at least 8,000 rpm. If
the fixed speed setting is below 8,000 rpm, you must press and hold the Silence
Alarm or Test Select button for a count of two in order to restart the pump.
Ausculate over the LVAD pocket to verify that the pump is running.
Cleaning Battery and Battery Clip Terminals
Dirty battery terminals may prevent proper battery charging, which can affect
battery operation. The metal terminals on the batteries and inside the battery
clips should be cleaned at least once a week with a Q-Tip™ or lint-free cloth that
has been dipped in rubbing alcohol (Figure 11).Allow the alcohol to dry before
using the batteries or clips, or before placing batteries into PBU battery charg-
ing slots.
CLINICAL OPERATION AND PATIENT MANAGEMENT
16
Figure 10 Battery Clip and Battery
Figure 11 Cleaning Metal Battery Contacts and Metal Contacts inside a Battery Clip.

Battery Fuel Gauge
The HeartMate II System Controller has a set of indicator lights, collectively called
the Battery Fuel Gauge . The Battery Fuel Gauge provides an approximate measure
of available battery power. More lights indicate more battery power; fewer lights
indicate less battery power (see Table 2 below).
To activate the Battery Fuel Gauge, press and hold the Silence Alarm button on the
System Controller keypad. Batteries should be changed when the battery fuel gauge
indicates 25% of power remains (one green light).
Battery Advisories and Alarms
Ye l lo w B a t te r y Ad v i s o r y
An illuminated YELLOW BATTERY symbol accompanied by a BEEP every four
seconds means that less than 15 minutes of battery power remains.
Action: Change batteries or switch to alternate power source (ie, PBU or EPP).
Red Battery Alarm
An illuminated RED BATTERY symbol and CONTINUOUS AUDIO TONE means
that less than 5 minutes of battery power remains.When this condition arises,
the LVAD automatically defaults to Power Saver Mode, gradually decreasing the
pump speed to 8,000 rpm. If, however, the previously selected speed is lower
than 8,000 rpm, the pump will remain at the low speed setting. Note: Patient's
may become symptomatic due to the drop in pump speed. The LVAS will remain
in Power Saver Mode until fully-charged batteries are installed, the PBU is con-
nected, or until no further power remains. Therefore, the RED BATTERY hazard
alarm prompts for an immediate response; an alternate power source must be
initiated. When the alarm condition clears, the LVAD will revert to the previous
fixed speed.
CLINICAL OPERATION AND PATIENT MANAGEMENT
17
Battery Fuel Gauge Meaning Response
75-100% of battery
power remains. No action needed.
50-75% of battery
power remains. No action needed.
25-50% of battery
power remains. No action needed.
Less than 25% of bat-
tery power remains.
Replace depleted bat-
teries with fully-charged
set or switch to PBU.
4 Green Lights
3 Green Lights
2 Green Lights
1 Green Light
Table 2 Battery Fuel Gauge Summary
Table of contents
Other Thoratec Medical Equipment manuals
Thoratec
Thoratec HeartMate III User manual
Thoratec
Thoratec CentriMag RVAS User manual
Thoratec
Thoratec PediMag User manual

Thoratec
Thoratec HEARTMATE II User manual
Thoratec
Thoratec HeartMate 3 Coring Tool User manual

Thoratec
Thoratec HeartMate 3 Coring Tool Instruction sheet
Thoratec
Thoratec HEARTMATE II User manual
Thoratec
Thoratec TLC-II User manual

Thoratec
Thoratec HeartMate III User manual

Thoratec
Thoratec HeartMate III Operating and safety instructions