en
Aesculap®
S4® Spinal System - Lumbar/Deformity
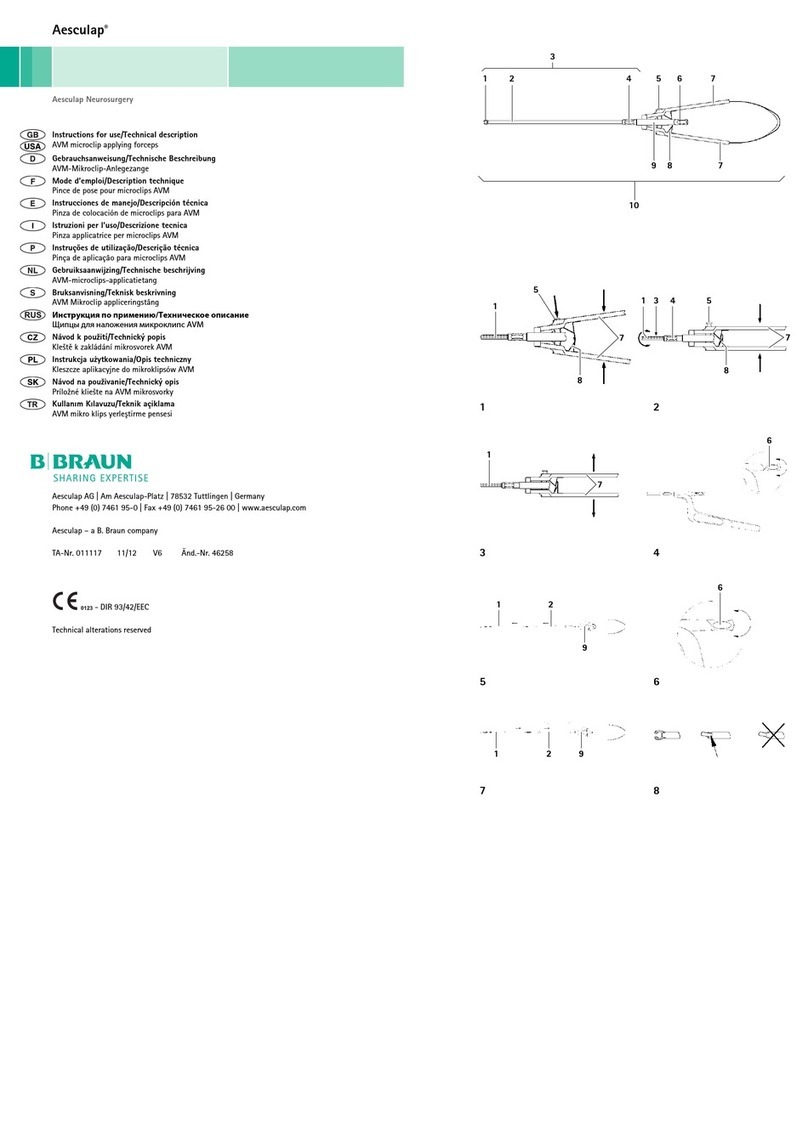
Legend
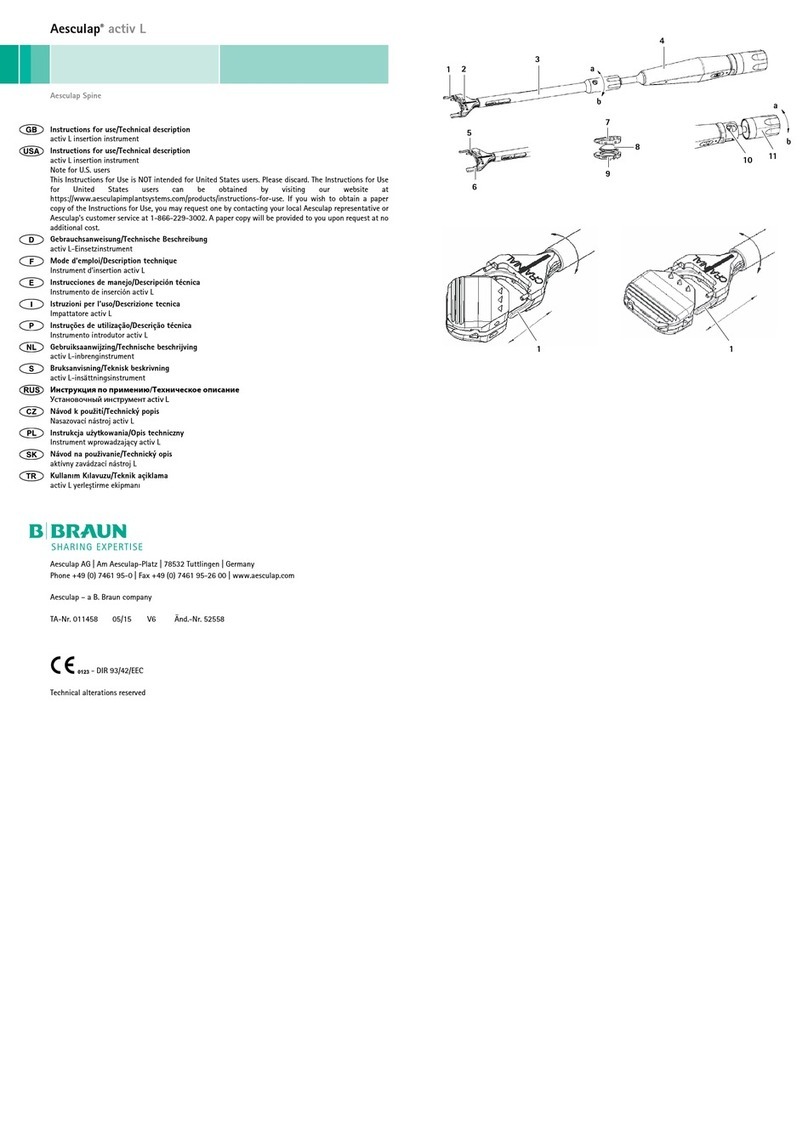
Fig. 1 S4monoaxial screws
Fig. 2 S4Element monoaxial screws
Fig. 3 S4polyaxial screws
Fig. 4 S4Element polyaxial screws
Intended use
The S4Spinal System-implants are used for dorsal monosegmental and multisegmental stabilization of the lumbar
and thoracic spine. They comprise:
■Mono/polyaxial screws
■Rods
■Hook
■Cross connector
■Rod connectors – parallel, axial and lateral offset
■appropriate fixation elements
Special instruments must be used for implanting these components, as well as for the distraction, compression and
reduction of the lumbar and thoracic spine.
Materials
The materials used in the implant are listed on the packaging:
■ISOTAN®Ftitanium forged alloy Ti6Al4V acc. to ASTM F136/ISO 5832-3
■ISOTAN®Ppure titanium acc. to ASTM F67/ISO 5832-2
The titanium implants are coated with a colored oxide. Slight changes in coloration may occur, but do not affect the
implant quality.
ISOTAN® is a registered trademark of Aesculap AG, 78532 Tuttlingen / Germany.
Indications
Surgically installed implants serve to support normal healing processes. They are not intended for use either as
replacements for natural body parts or to bear loads over the long term in the event the healing process is incomplete
or slow.
Use for acute disorders of the spine that cannot be treated by other therapies:
■Fractures
■Pseudarthrosis or delayed healing
■Dislocation
■Degenerative instability
■Post-discectomy syndrome
■Spondylolisthesis
■Kyphosis
■Scoliosis
■Stenosis
■Post-trauma instability
■Tumors
■Osteoporosis (with the simultaneous use of bone cement and fenestrated screws)
Absolute contraindications
Do not use in the presence of:
■Severe damage to the bone structures of the spine that could prevent the stable implantation of the implant
components; for example, osteopenia, severe osteoporosis, Paget’s disease, bone tumors etc.
■Metabolic or degenerative metabolic bone diseases that could compromise the stable anchoring of the implant
system
■Suspected allergy or sensitivity to the implant materials
■Acute or chronic vertebral infections of a local or systemic nature
■Poor patient compliance or limited ability to follow medical instructions, particularly in the post-op phase,
including with regard to the restrictions on range of movement in terms of physical exercise and occupational
activity
■Cases not listed under indications
Relative contraindications
In the following circumstances, use of the implant system could represent an increased clinical risk and therefore
requires precise, individual assessment by the surgeon:
■Medical or surgical conditions that could negatively impact the success of the implantation, including wound
healing disorders
■Conditions that could subject the spine and implants to excessive pressure,
■for example, pregnancy, obesity, neuromuscular diseases or disorders
■Generally poor condition of the patient; for example, drug or alcohol addiction
Side effects and interactions
The general risks of surgery are assumed known and are therefore not described in these instructions for use. Poten-
tial risks and clinical consequences associated with use of the implant system include, but are not limited to:
■Implant failure resulting from excessive load
– Warping or bending
– Loosening
–Breakage
■Poor stabilization, requiring subsequent revision surgery or surgery to remove the implant system
■Failed or delayed fusion
■Infection
■Fractured vertebral body or bodies
■Tissue reaction to implant materials
■Hematomas and wound healing disorders
■Injuries to
– Nerve roots
– Spinal cord
– Blood vessels
–Organs
■Changes of the normal spine lordosis
■Neurological disorders, including impairment of the gastrointestinal, urological and/or reproductive system
■Pain or indisposition
■Bursitis
■Decreased bone density due to load avoidance
■Bone atrophy/fracture above or below the spine section provided for
■Limited physical ability
■Persistence of symptoms that were to be treated by the implantation
■Paresis
■Subsequent surgery to remove the implant system
■Metal/foreign body allergy or hypersensitivity
■Dural tears
■Meningitis
Safety notes
■It is the operating surgeon's responsibility to ensure that the surgical procedure is performed properly.
■General risk factors associated with surgical procedures are not described in this documentation.
■The operating surgeon must have a thorough command of both the hands-on and conceptual aspects of the
established operating techniques.
■The operating surgeon must be fully conversant with bone anatomy, including the pathways of nerves, blood ves-
sels, muscles, and tendons.
■The operating surgeon is responsible for combining and implanting the implant components, with or without
bone cement.
■Aesculap is not responsible for any complications arising from erroneous indication, wrong choice of implant,
incorrect combination of implant components and operating technique, the limitations of the treatment method,
or inadequate asepsis.
■The instructions for use of the individual Aesculap implant components and instruments must be observed.
■The implant components were tested and approved in combination with Aesculap components. If other combi-
nations are used, the responsibility for such action lies with the operating surgeon.
■Do not, under any circumstances, combine implant components from different manufacturers.
■Do not, under any circumstances, use damaged or surgically excised components.
■Implants that have been used before must not be reused.
■Delayed healing can cause implant breakage due to metal fatigue.
■The attending physician shall make any decision with regard to the removal of implant components that have
been used,
■Damage to the load-bearing structures of the implant can lead to loosening of components, dislocation, migra-
tion, and other severe complications.
■To ensure the earliest possible detection of such causes of dysfunction, the implant must be checked periodically,
using appropriate techniques.
■The implant components applied, along with their article numbers, the name of the implant, as well as the batch
number and serial number (if available) must be documented in all patient records.
■Postoperatively, individual patient information, as well as mobility and muscle training, is of particular impor-
tance.
Sterility
■The implant components are supplied in an unsterile condition.
■The implant components are packaged individually.
►Store implant components in their original packaging and remove from their original protective wrapping only
immediately prior to processing.
►Use a suitable tray for cleaning/disinfection.
►Ensure that the implant components in their implant system storage devices do not come into contact with each
other or with instruments.
►Ensure that the implant components are not damaged in any way.
Prior to initial sterilization and subsequent resterilization, the implant components must be cleaned using the fol-
lowing validated reprocessing procedure:
Note
Adhere to national statutory regulations, national and international standards and directives, and local, clinical
hygiene instructions for sterile processing.
Note
For patients with Creutzfeldt-Jakob disease (CJD), suspected CJD or possible variants of CJD, observe the relevant
national regulations concerning the reprocessing of products.
Note
Successful processing of this medical device can only be ensured if the processing method is first validated. The oper-
ator/sterile processing technician is responsible for this.
The recommended chemistry was used for validation.
Note
For up-to-date information about reprocessing and material compatibility, see also the Aesculap Extranet at
https://extranet.bbraun.com
The validated steam sterilization procedure was carried out in the Aesculap sterile container system.
Validated reprocessing procedure
Cleaning/Disinfection
Validated cleaning and disinfecting procedure
WARNING
Risk of screw breakage caused by pedicle screws used for spondylolisthesis!
►Support the stabilization measure with an intercorporal fusion (ALIF, PLIF or
TLIF).
WARNING
The implant has not been evaluated for safety and compatibility in the MR envi-
ronment. It has not been tested for heating, migration or image artifact in the MR
environment. Scanning a patient who has this implant may result in patient injury.
WARNING
Intraoperative contamination with blood, secretions, and other fluids may render
the affected component unsuitable for resterilization!
►Handle the implants with new gloves only.
►Keep the implant system storage devices covered or closed.
►Process implant system storage devices separately from instrument trays.
►Clean implants must not be processed together with contaminated implants.
►Process the implant components individually and separately if no implant sys-
tem storage devices are available, ensuring that the implant components are
not damaged in the process.
►Do not reuse surgically contaminated implants!
WARNING
Direct or indirect contamination may render implants unsuitable for resteriliza-
tion!
►Do not reprocess implants that have been directly or indirectly contaminated
with blood.
Validated procedure Specific requirements Reference
Manual cleaning with immersion
disinfection
■SW790T
■Do not clean with brushes or
other abrasives that would
damage the product surface.
■To prevent internal stresses and
weakening of the implants,
avoid scoring or scratching any
components.
Chapter Manual cleaning/disinfec-
tion and sub-chapter:
■Chapter Manual cleaning with
immersion disinfection