This document is valid only on the date printed. If unsure of the print date, please
re-print to ensure use of the latest revision of the IFU (available at www.e-ifu.com).
The onus resides with the user to ensure that the most up-to-date IFU is used. 8 of 12
3. Postoperative care is extremely important. The patient must
be instructed in the limitations of the metallic implant and be
warned regarding weight bearing and body stresses on the
appliance prior to firm bone healing. The patient should be
warned that noncompliance with postoperative instructions
could lead to failure of the implant and possible need thereafter
for additional surgery to remove the device.
4. During the application of the cement, radiological control is
essential so that the operator can follow the progress of the
filling and stop the procedure if the slightest leakage of cement
is detected. Use appropriate imaging techniques such as
fluoroscopy or CT imaging guidance to confirm correct needle
placement, absence of damage to surrounding structures
and appropriate location of injected cement. Imaging, such
as venography, may also be used to assess the ability of the
vertebra to contain the injected cement.
5. If surgeon chooses to complete a biopsy prior to screw
placement, care should be taken not to place the tip of the
biopsy needles beyond the desired location of the screw tip in
order to reduce leakage or extravasation risk.
6. EXPEDIUM Fenestrated Screws System implants and
instruments must never be reused. An explanted implant
should never be reimplanted. Even though a device appears
undamaged after explanting, it may have small defects and
internal stress patterns that may lead to early breakage. Reuse
of single use implants and instruments may compromise
instrument performance and patient safety and can also cause
cross-contamination leading to patient infection.
PROCEDURE
CAUTION: It is essential to maintain strict sterile technique
during the procedure and during all phases of handling
this product.
1. Place each EXPEDIUM Fenestrated Screw into the pedicle
per the EXPEDIUM Spinal System Surgical Technique
Manual for proper screw insertion steps. It is critical that
NO torsion movement should be applied to the screw after
injecting the cement).
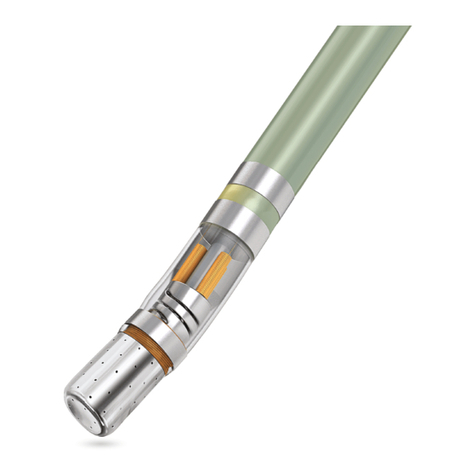
2. Thread the Cannula into the Clip.
3. Mix the spinal cement of choice (CONFIDENCE Spinal
Cement, VERTEBROPLASTIC Radiopaque Resinous Material
or VERTECEM V+ Cement) per the instructions provided in
the package inserts. Follow the time temperature chart from
respective cement package insert very carefully not to exceed
the working time.
4. If CONFIDENCE Spinal Cement is used, CONFIDENCE
Spinal Cement Delivery System must be attached to the
threaded connection of the EXPEDIUM Fenestrated Screw
Clip-on Delivery Device (Cannula and Clip). If V-MAX
Mixing and Delivery Device is used, it should be attached to
the CONFIDENCE Needle Adapter, which should then be
attached to the Clip-on Delivery Device.
5. Place the Clip-On Delivery Device through the screw head
and into the bone shank. Once the Cannula is inside the
shank, the Clip will engage the screw head.
6. Follow instructions from package inserts of the CONFIDENCE
SPINAL CEMENT SYSTEM, the V-MAX Mixing and Delivery
Device, or the VERTECEM V+ Cement Kit to introduce the
cement through the EXPEDIUM Fenestrated Screw Cannula.
7. Use Fluoroscopic or CT imaging guidance throughout the
procedure to verify and monitor cement flow as appropriate.
8. When the appropriate amount of cement has been introduced,
stop cement introduction as indicated per the manufacturers
technique. It is recommended not to exceed 2cc of cement
per pedicle in order to reduce the occurrence of cement
leakage and extravasation. Un-engage the Clip-On Delivery
Device from the screw head and remove it from the screw.
9. Place the Clip-on Delivery Device into the next screw per step
5, and follow steps 5-7 as working time permits (follow the
time temperature chart from respective cement package insert
very carefully not to exceed the working time).
10. Repeat this process for each screw if desired. Prior to the
completion of the working time, the Clip-on Delivery Device
should be removed from the screw, and a new Cannula
should be utilized with a new package of cement and cement
delivery system (either the CONFIDENCE SPINAL CEMENT
SYSTEM, the V-MAX Mixing and Delivery Device and the
VERTEBROPLASTIC Radiopaque Resinous Material, or the
VERTECEM V+ Cement Kit) for next levels (follow steps 3-7).
IMPORTANT PHYSICIAN INFORMATION
1. EXPEDIUM Fenestrated Screw System, like any other temporary
internal fixation devices, has a finite useful life. The patient’s
activity level has a significant impact on this useful life. Your
patient must be informed that any activity increases the risk of
loosening, bending, or breaking of the implant components.
It is essential to instruct patients about restrictions to their
activities in the postoperative period and to examine patients
postoperatively to evaluate the development of the fusion mass
and the status of the implant components. Even if solid bone
fusion occurs, implant components may nevertheless bend,
break, or loosen. Therefore, the patient must be made aware
that implant components may bend, break, or loosen even
though restrictions in activity are followed.